HIATAL HERNIAS AND ABDOMINAL WALL HERNIAS: PREDICTORS OF ASSOCIATION IN A LARGE COHORT OF PATIENTS
Nisarg Mehta*1, Shahin Ayazi1,2, Sven Eriksson1, Margaret Riccardi1, Kirsten Newhams1,2, Ping Zheng1, Christine Delfino1, Blair Jobe1,2
1Esophageal Institute , Allegheny Health Network, Pittsburgh, PA; 2Drexel University, Philadelphia, PA
Introduction:
Risk factors for abdominal /groin hernias have been well studied and appear to overlap with those for hiatal and paraesophageal hernia (HH/PEH). This suggests a potential association between these two categories of hernia. However, no large studies have examined such an association. We designed the current study to characterize this association and identify factors associated with this coexistence.
Methods:
A database of patients seen at a large multi-center health network serving 3 states in the mid-Atlantic region of the United States was queried for patients aged 18-95 with a BMI of 16-80 and a documented diagnosis of HH/PEH. This sample population was then queried for a diagnosis of an additional hernia (ventral, inguinal/ femoral, umbilical or incisional hernia). Demographic data (sex, age and BMI) and comorbidities [tobacco use, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), hypertension (HTN), obstructive sleep apnea (OSA), diabetes mellitus (DM), hyperthyroid and hypothyroid] were collected to assess for impact on the presence of additional hernias. Demographics and comorbidities of the group of patients with and without additional hernia along with hiatal hernia were then compared using univariate, followed by multivariate logistic analysis.
Results:
The final study population consisted of 28,852 patients (66.5% female) with HH/PEH. The prevalence of an additional hernia in this population was 8.2% (n=2299). Of these 69.1% had only one additional hernia with the remaining 30.9% having two or more additional hernias. The most common type of additional hernia was ventral (50.5%), followed by inguinal (36.4%), umbilical (29.8%) and incisional (20.4%).
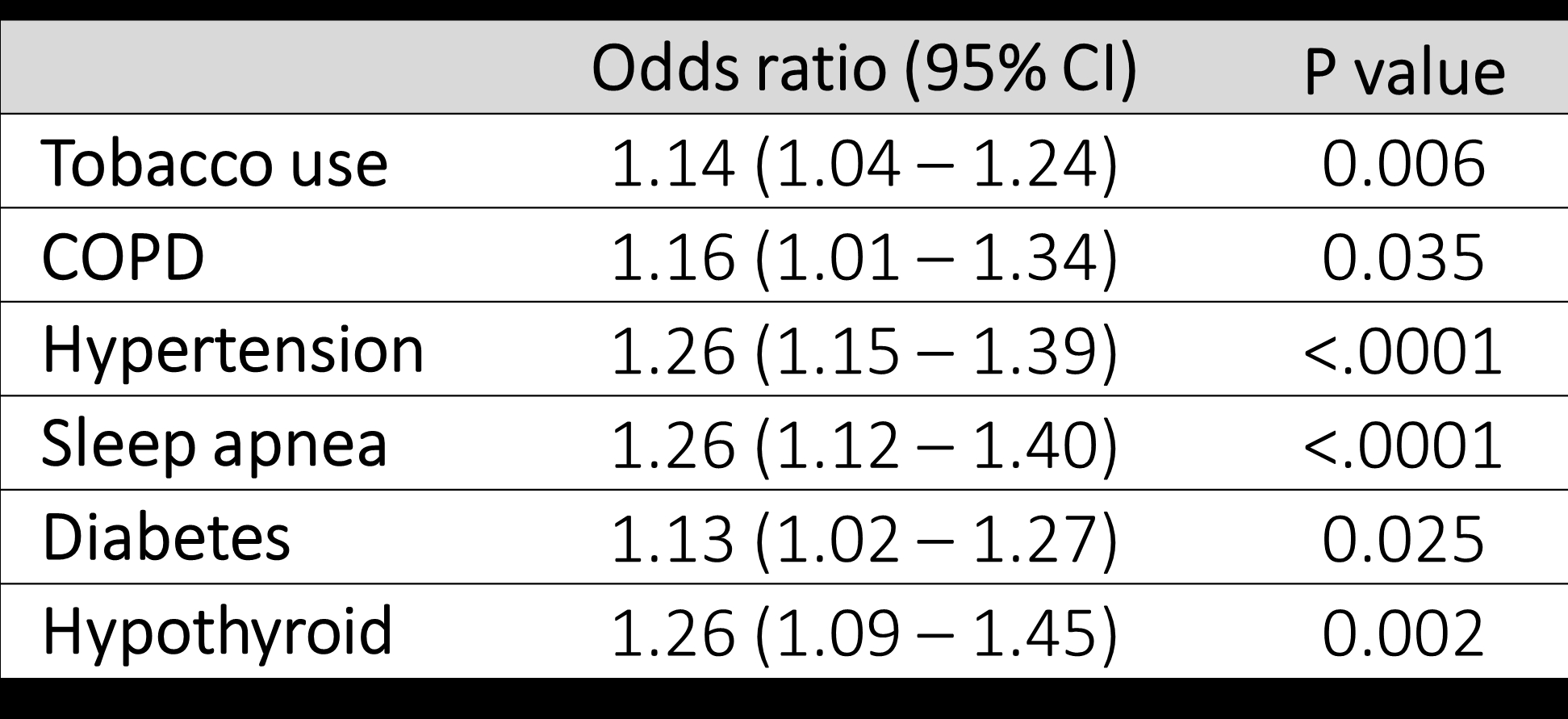
Male patients with PEH/HH were more likely to have an additional hernia [OR: 2.0 (CI: 1.83 – 2.18), p< 0.0001]. This was also true for obese patients (BMI > 35) [OR: 1.25 (CI: 1.128 – 1.395), p<0.0001]. There was a stepwise increase in the odds ratio for presence of additional hernia with each decade of life over 30 with peak at 60-69 [OR: 6.9 (3.45, 14.10) (Figure 1). The co-morbidities found to be predictors of association between HH/PEH with other types of hernia are shown in figure 2. BPH [OR: 2.00 (CI: 1.64 – 2.44), p< 0.0001] and CKD [OR: 1.55 (CI: 1.23 – 1.95), p = 0.0002] were found to be significant factors only on univariate analysis, but not on multivariate analysis.
Conclusion:
The prevalence of an additional hernia in patients with a HH/PEH was 8.2%. Although HH/PEH are more prevalent in females, males with HH/PEH are at higher risk for additional hernias. There is a stepwise increase in the risk of additional hernias with increase in each decade of life. Obesity, tobacco use, COPD, HTN, OSA, DM and hypothyroidism are independent risk factors for presence of additional hernias.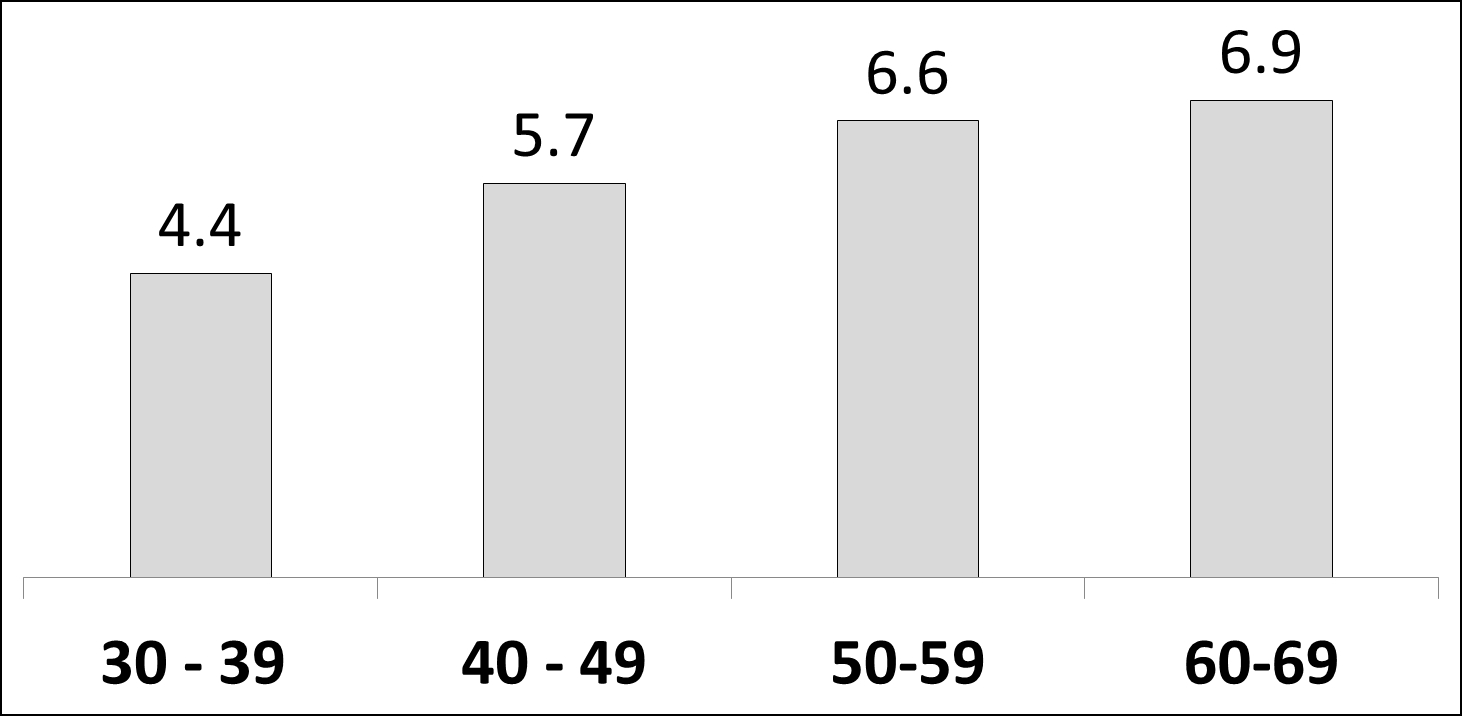
Back to 2022 Posters
