NOVEL STRATEGY OF TWO STAGE HEPATECTOMY COMBINED WITH 90Y RADIOEMBOLIZATION FOR MULTIPLE BILOBAR COLORECTAL LIVER METASTASES
Tadahiro Uemura*, Lorenzo Machado, Aaron Dunn, Brian Thomas, Andrew klobuka, Rachel Tindall, Ngoc Thai
Allegheny Health Network, Pittsburgh, PA
Background: Multiple bilobar colorectal liver metastases are challenging diseases for liver resection. Portal vein embolization (PVE) or associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) are currently used to increase functional liver remnant (FLR). However, in traditional two stage hepatectomy, up to a third of patients are unable to proceed to the second stage due to disease progression or failure of the FLR to achieve adequate hypertrophy while the ALPPS procedure is associated with increased morbidity and mortality. Furthermore, we also experienced severe adhesion around the hepatic hilum during the second stage as a result of the hepatoduodenal ligament dissection during the first stage of hepatectomy. Therefore, we used 90Y radioembolization to increase FLR, prevent tumor growth and facilitate the second stage of hepatectomy.
Patient: A patient was 68 year old female who had colon cancer with synchronous bilobar liver metastases (pT4 pN1b pM1b stage IVB). She underwent laparoscopic left hemicolectomy for primary lesion and received 13 cycle of FOLFOX plus bevacizumab and 10 cycles of FOLFIRI plus bevacizumab. During the course of adjuvant chemotherapy, total 7 lesions of bilobar liver lesions were stable and she was referred to liver resection. Treatments as follows:
Stage 1 hepatecotomy : Robotic laparoscopic partial liver resection of segment 3 and 4
Three weeks later
90Y radioembolization for right lobe of liver (dose of 120 mCi )
Eleven weeks later
Stage 2 hepatectomy: Right trisectionectomy of liver
The initial FLR was 241 cc (16% of total liver volume) and it increased to 403 cc (30% of total liver volume) following 90Y radioembolization (Figure 1). The CEA was 27.7 ng/mL prior 90Y radioembolization and down to 3.8 ng/ml post 90Y radioembolization. The second stage of hepatectomy achieved R0 resection and the pathological finding showed multiple nodules of metastatic colorectal adenocarcinoma with varying degree of treatment related necrosis (Figure 2). The patient's postoperative course was uneventful and no evidence of recurrence in liver on short term follow up.
Discussion: 90Y radioembolization can be used to increase FLR significantly and control the liver disease during the waiting period. Liver resection can then be safely performed following 90Y radioembolization. Utilization of 90Y radioembolization combined with staged hepatectomies can be useful strategy for multiple bilobar liver metastases.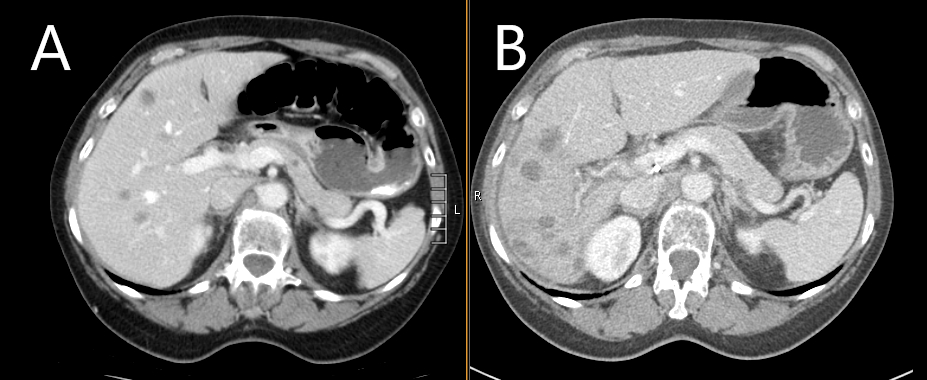
Figure 1A: Prior 90Y radioembolization, Figure 1B: Post 90Y radioembolization, significant hypertrophied left lateral segment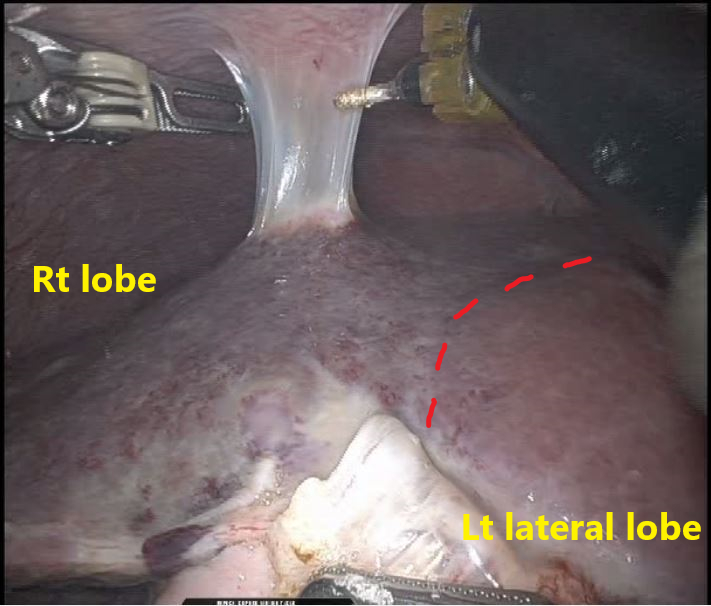
Figure 2: Discolored and atrophied right lobe treated with 90Y radioembolization, well perfused and hypertrophied left lateral lobe
Back to 2022 Posters
