A 20-YEAR EXPERIENCE IN OVER 200 CASES WITH GIANT PARA-OESOPHAGEAL HERNIA REPAIR WITH CRURAL REPAIR AND GASTROPEXY BUT WITH SELECTIVE ANTI-REFLUX PROCEDUE.
Priyantha Siriwardana1, Alan Askari*1, Etsuro Yazaki2,3,1, Bruno Lorenzi1, Alex Charalabopoulos4,1, Mohammad Qamruddin1, Sritharan Kadirkamanathan1,3
1Upper GI Surgery, Broomfield Hospital, Chelmsford, Essex, United Kingdom; 2Wingate Institute of Neurogastroenterology, London, United Kingdom; 3Queen Mary University of London Barts and The London School of Medicine and Dentistry, London, London, United Kingdom; 4Laiko Geniko Nosokomeio Athenon, Athens, Attica, Greece
Background: Para-oesophageal (PEH) hernia or so called "large hiatus hernia" is less common but is more cause for concern if they are symptomatic. They may present with post-prandial pain (chest pain or upper abdominal) or vomiting, shortness of breath or difficulty swallowing or reflux related symptoms. Symptomatic PEHs are usually repaired electively as they are at higher risk for progressing to incarceration or ischemia resulting in the need for emergency surgery. In addition, PEH appears to be associated with anaemia too.
PEH is common in elderly, but there is general reluctant to refer for surgery. Controversy persists as to the surgical approach, and it is debatable whether an anti-reflux procedure is required at the same time as PEH Repair (PEHR).
Aim: Objective is to evaluate our management and outcomes of giant- PEHR for the last 20 years.
Methods: A retrospective analysis of prospectively collected data of patients that underwent surgery for PEH from January 2001- June 2021 was performed. Clinical presentation, management including pre-operative investigations and evaluation, post-operative clinical outcomes, haemoglobin (Hb) level, respiratory function {Forced Vital Capacity (FVC), Forced Expiratory Volume in 1 Second (FEV1)}, radiographic evaluation and quality-of-life (QoL) with SF-36 questioners were assessed.
Results: 202 patients (122 females) with median age of 68 years (range 36-88) underwent surgery for PEH. The main presenting symptom was shortness of breath in 81 (40%). Ninety-five (47%) were ASA III , 119 (59%) had microcytic anaemia. At PEHR, the hernial sac was dissected before reduction of contents, and the hiatus was reconstructed in all the patients with crural closure. A mesh was rarely used. A gastropexy was performed. Patients with reflux were evaluated objectively and a fundoplication (Nissen or Toupet) was performed in only 142 (70%) of the patients during PEHR. Median hospital stay was significantly lower in laparoscopic group; 4 days (1-16) compared to open of 10 days (5-33). Thirty-day mortality was 1% (2/202). Median follow-up was 10 years. Symptoms improved in 166 (82%). Shortness of breath improved remarkably and was objectively assessed with respiratory function tests. Post-operative haemoglobin levels improved significantly in those who were anaemic. (Table 2). QoL scores (general health, physical, emotional, and social components) improved significantly following Giant PEHR. 42(21%) had radiological recurrences but only nine (4.5%) clinical recurrence requiring surgery.
Conclusions
Laparoscopic repair of giant PEH with crural repair plus gastropexy but with selective anti-reflux procedure is safe with good outcomes in all age groups with improvement in QoL, respiratory function and associated anaemia. Reflux should be evaluated pre-operatively, and if present, a fundoplication should be considered at PEHR.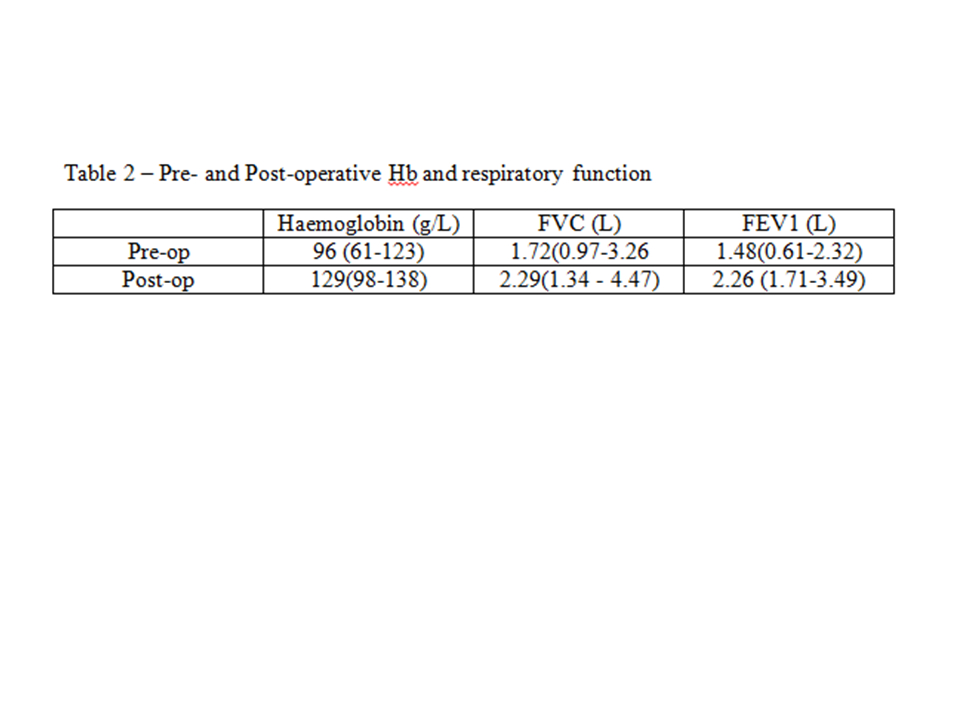
Back to 2022 Abstracts
