A NOVEL, LARGE ANIMAL ISCHEMIC MODEL FOR ESOPHAGOGASTRIC ANASTOMOSIS USING INDOCYANINE GREEN (ICG) ANGIOGRAPHY
Jennifer Williams*, Andrew Lin, Brian Zilberman, Connor Crudeli, Julieta E. Barroeta, Francis Spitz, Jennifer M. Burg, David Shersher
Surgery, Cooper University Health Care, Camden, NJ
Background
The construction of a well perfused esophagogastric anastomosis is critical to avoid the most morbid complication of esophagectomy, anastomotic leak. Utilization of ICG provides an objective measurement of tissue perfusion. We describe a reproducible protocol for the construction of both ischemic and non-ischemic esophagogastric anastomoses in swine using ICG.
Methods
Eight pigs underwent an abdominal-approach distal esophagectomy, creation of a gastric conduit, and esophagogastric anastomosis. The pigs were divided into two groups, non-ischemic (perfusion >65%) and ischemic (perfusion 50-60%). The pigs were euthanized at 7 or 14 day endpoints. Postoperative courses and weights were recorded. At necropsy, the anastomosis was evaluated grossly and histologically.
Results
The three pigs with non-ischemic anastomoses all had uneventful postoperative courses and intact anastomoses on necropsy. The three pigs with ischemic anastomoses all had sepsis requiring antibiotics. Two of three had a disrupted anastomosis on necropsy and two of three had dense adhesions of the anastomosis to the liver. At 14 days the non-ischemic pigs gained weight and ischemic pigs lost weight. On pathologic examination, acute inflammation was greater at 7 days than 14 days and no difference was seen in ischemic vs. non-ischemic anastomotic histology. Two pigs died prematurely during protocol development and were not included in the results as outcomes could not be measured.
Conclusions
We demonstrate the feasibility and reproducibility of using ICG perfusion technology to create an ischemic esophagogastric anastomosis in a large animal model. We aim to use this animal model to evaluate intraoperative interventions on at-risk anastomoses with the goal of reducing or preventing anastomotic leaks.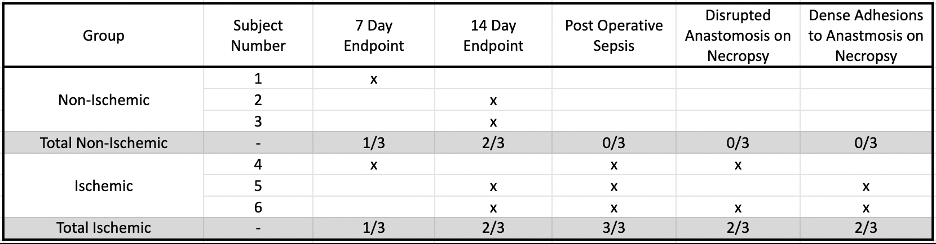
Table 1: Postoperative summary for the 6 pigs included in the study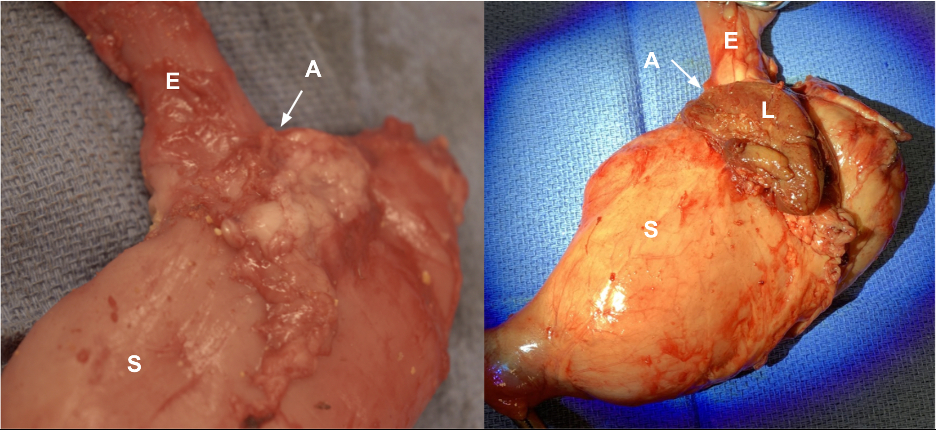
Image 1: Representative images of the gross pathology on necropsy.
Key: E=esophagus, A= anastomosis, S=stomach, L=Liver tissue
Left: Non-ischemic anastomosis at 14 days with no major adhesions
Right: Ischemic anastomosis at 14 days with liver densely adherent to anterior anastomosis
Back to 2022 Abstracts
