EXTENSIVE COLITIS AND CURRENT OR FORMER SMOKING ARE ASSOCIATED WITH POST-OPERATIVE COMPLICATIONS WITHIN 30 DAYS OF ILEAL POUCH-ANAL ANASTOMOSIS FOR ULCERATIVE COLITIS IN A STATE-LEVEL REGISTRY
Edward L. Barnes*1, Scott Esckilsen1, Jean Ashburn2, Amy Barto3, Richard S. Bloomfeld2, Ashley Cairns2, Kurren Mehta3, Pooja Patel3, Jennifer Dziwis3, Reza Rahbar4, Timothy S. Sadiq4, John S. Hanson5, Hans Herfarth1
1University of North Carolina School of Medicine, Chapel Hil, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC; 3Duke University School of Medicine, Durham, NC; 4University of North Carolina System, Chapel Hill, NC; 5Atrium Health, Charlotte, NC
Background: Our understanding of outcomes after proctocolectomy with ileal pouch-anal anastomosis (IPAA) for ulcerative colitis (UC) is largely based on single-center evaluations or analyses of selected populations. We aimed to create a state-level registry to evaluate the epidemiology of IPAA surgery and pouch-related outcomes across the major healthcare systems performing these surgeries in our state.
Methods: We created a retrospective cohort of all patients undergoing restorative proctocolectomy with IPAA for UC at one of four centers in our state between January 1, 2018 and December 31, 2020. The primary outcomes of this study were the rate of complications and all-cause readmissions within the first 30 days of the final stage of IPAA surgery. Complications were defined as development of a peri-pouch abscess, pelvic sepsis, documented leak, urinary tract infection, Clostridioides difficile infection, other surgical site or wound infection, or ileus within the 30 days of surgery. We also evaluated the rate of venous thromboembolic events and need for re-operations during this time period. Complications were assessed individually and as a composite outcome. Bivariate and multivariable logistic regression were used to compare clinical and demographic characteristics that may be associated with these primary outcomes.
Results: During the study period, 170 patients underwent IPAA surgery with 64 (38%) experiencing a complication within 30 days. In bivariate analysis, patients with extensive disease and patients who were current or former smokers were more likely to experience a complication (Table 1). The use of preoperative therapies including biologic and small molecule therapies was not associated with an increased risk of complications or readmission. After adjusting for the number of stages in IPAA surgery, patients with extensive UC (OR 3.41, 95% CI 1.32 – 8.85) were more likely to experience a complication compared to patients with left-sided colitis or proctitis (Table 2). Patients who were current or former smokers were also more likely to experience a complication (OR 3.44, 95% CI 1.58 – 7.52). Among all patients, 56 (33%) required readmission within 30 days. The most common reasons for readmission were ileus/small bowel obstruction (21%), peri-pouch abscess (18%), and dehydration (16%).
Conclusion: In this first state-level examination of the epidemiology of IPAA for UC, we demonstrated that the complication rate after IPAA for UC was approximately 38%, with one-third of patients being readmitted within 30 days. Extensive disease at the time of colectomy appears to be an indicator of more severe disease and may portend a worse prognosis after IPAA. This resource will provide the infrastructure for future studies of the natural history after IPAA at the state level.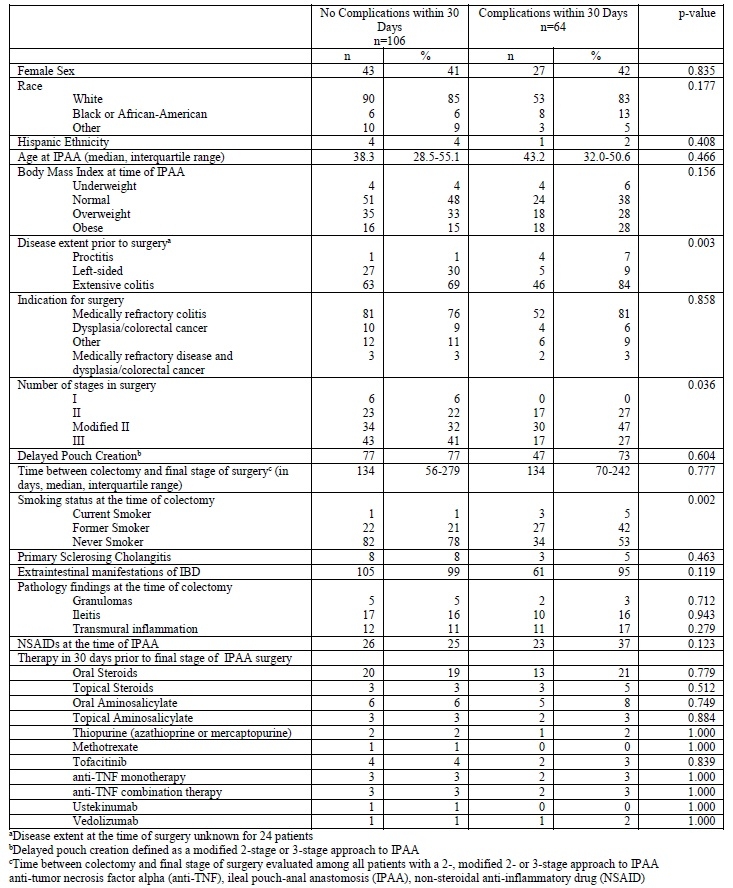
Table 1. Comparison of demographic and clinical characteristics among patients who experienced a complication within 30 days of ileal pouch-anal anastomosis for ulcerative colitis and patients who did not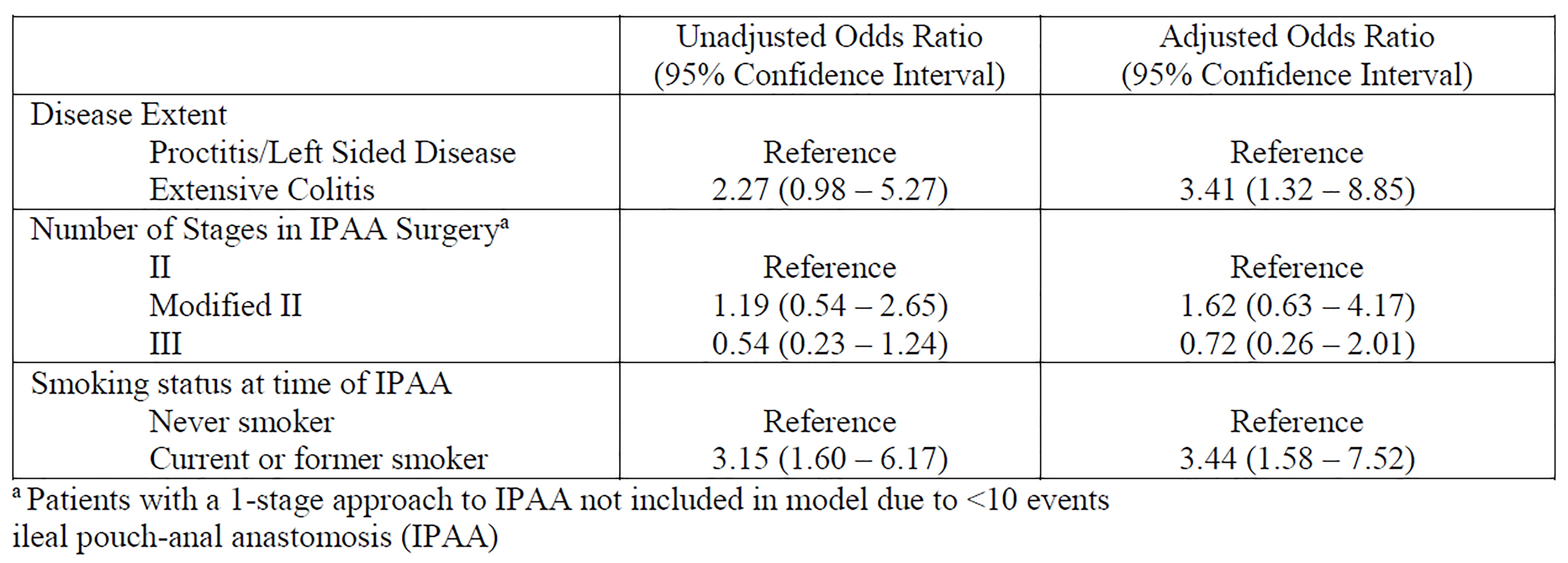
Table 2. Odds of developing a complication within the first 30 days of ileal pouch-anal anastomosis for ulcerative colitis after adjusting for potential risk factors
Back to 2022 Abstracts
