DELAYED REFERRAL TO CRS/HIPEC ASSOCIATED WITH DECREASED SURVIVAL FOLLOWING MALIGNANT PERITONEAL MESOTHELIOMA DIAGNOSIS: A MARKOV DECISION ANALYSIS
Armaun D. Rouhi*1, Gerard D. Hoeltzel2, Felix Ho3, Yanik J. Bababekov3, Arthur Yule3, Rashikh Choudhury3, Kristoffel Dumon1, Giorgos C. Karakousis1,4
1Department of Surgery, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA; 2Department of Surgery, Thomas Jefferson University Hospital, Philadelphia, PA; 3Department of Surgery, University of Colorado Hospital, Aurora, CO; 4Abramson Cancer Center, Philadelphia, PA
Introduction: Malignant Peritoneal Mesothelioma (MPM) remains a dire diagnosis with historically limited treatment options. Increasingly, patients have been referred for Cytoreductive Surgery with Hyperthermic Intraperitoneal Chemotherapy (CRS/HIPEC) in the setting of promising long-term survival reported for single center case series. As controversy exists as to the efficacy of CRS/HIPEC, delays for referral to a HIPEC center are common, particularly in rural regions in the United States. As such, it is unclear to what degree delay for referral for CRS/HIPEC impacts patient survival.
Methods: A decision-analytic Markov state transition model was created to simulate the life of MPM patients who were deemed eligible for CRS/HIPEC. Life expectancy following No Surgery, Immediate CRS/HIPEC, and Delay to Surgery (1-24 weeks following diagnosis) was estimated. Base case patients were defined as being a 50-year-old female with epithelioid subtype of MPM. Sensitivity analysis of time of delay (weeks) was performed. Markov parameters were extracted from literature review.
Results: Delayed referral for CRS/HIPEC was associated with reduced long-term patient survival. Immediate CRS/HIPEC improved survival compared with both No Surgery and Delay to Surgery groups. Base case patients who underwent immediate CRS/HIPEC gained 3.2 additional mean years of life compared with patients who underwent No Surgery. Patients experienced reduced survival with delayed referral, an effect which was potentiated with increased delay time.
Conclusion: Delay to CRS/HIPEC was associated with reduced long-term survival for operable MPM patients. Referral to HIPEC center should be done in expeditious manner to promote patient education and autonomy regarding their surgical treatment options.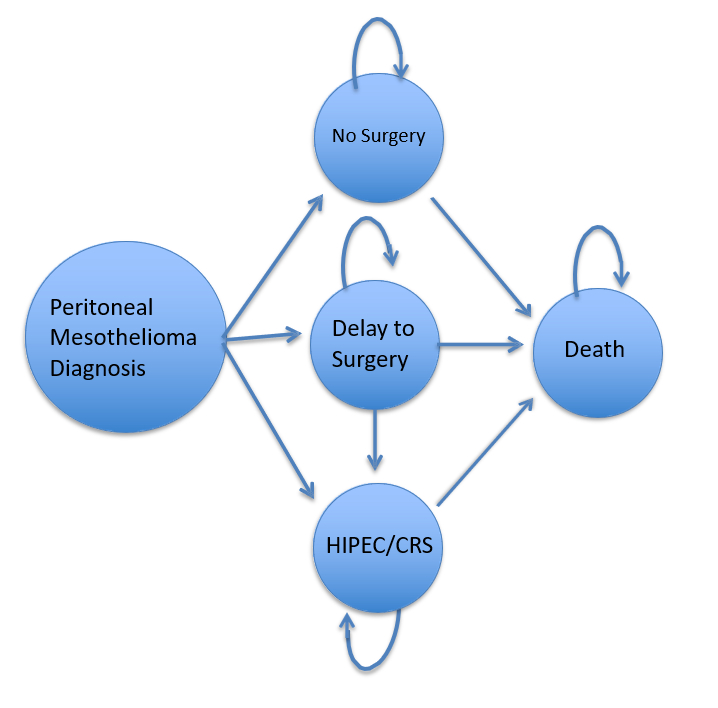
Decision model diagram. Three patient groups were created: No Surgery, Immediate CRS/HIPEC, and Delay to Surgery.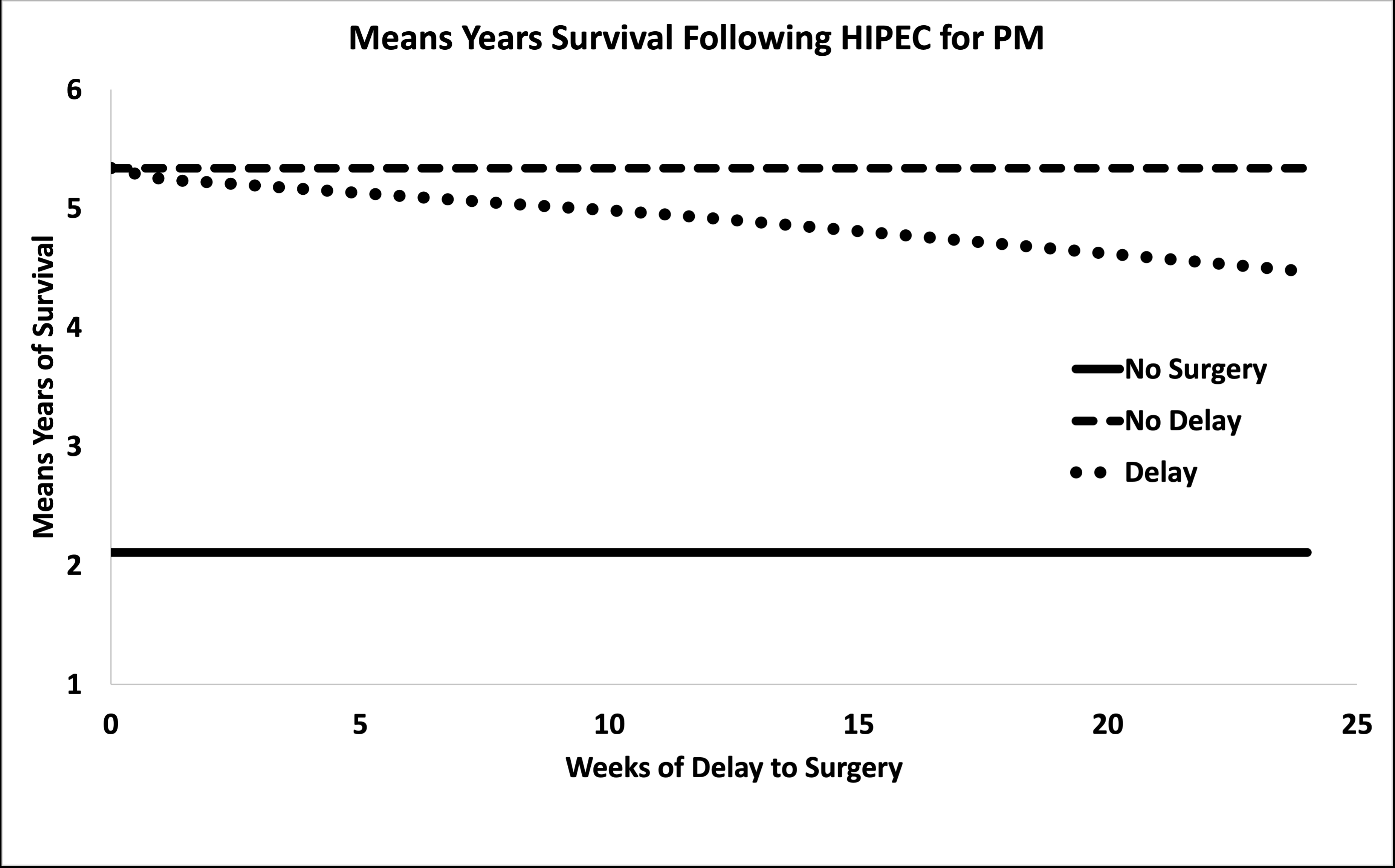
Time of delay sensitivity analysis
Back to 2022 Abstracts
