NECROTIZING FASCITIIS OF FLANK AND HIP WITH PELVIC ABSCESSES CAUSED BY MISSED SILENT APPENDICITIS: A RARE PRESENTATION.
Vishal Chandel*1, Imran Khokhar1, Sridhar Reddy Patlolla1, Jan Pasternak2, Joseph Demidovich1, Dominic Bontempo1, Matthew S. Mathew1
1Suburban Community Hospital, East Norriton, PA; 2Philadelphia College of Osteopathic Medicine, Philadelphia, PA
INTRODUCTION:
Acute appendicitis is one of the most common surgical condition. Necrotizing fasciitis is a rare infection of the deeper layers of skin and subcutaneous tissues, rapidly spreading across fascial planes within the subcutaneous tissue with an average mortality rate of 20.6% and is a surgical emergency. Necrotizing fasciitis due to perforated appendicitis is even rarer.
METHODS:
We present a case of necrotizing fasciitis of abdominal wall and right flank extending to hip secondary to a perforated appendix and reviewed the available literature. Confusion with cellulitis, can delay aggressive therapy.
CASE PRESENTATION:
A 66-year-old female presented with severe right flank and hip pain following 2-weeks history of right abdominal pain. She had tachycardia and hypotension. On physical examination, she had a large necrotic wound in right flank and hip with pus and blistering, and abdomen had no peritoneal signs. Her laboratory investigations revealed white cell count of 35,500/mm3. Non-contrast CT (patient was allergic to contrasts) showed features of necrotizing fasciitis in the flank and hip with inflamed and walled-off cecum and appendix. Antibiotics were started and emergent surgery revealed grossly necrotic tissue with multiple pockets of pus in subcutaneous tissue, fascia, and muscles of flank and hip extending to retroperitoneum along with multiple pelvic abscesses. Due to walling-off, disseminated retroperitoneal and pelvic infection had no further intraperitoneal connection. Her wound cultures grew Bacteroides, E.Coli and Aerococcus. Patient was discharged once stable, on wound vac and extended antibiotic regimen.
DISCUSSION:
Necrotizing fasciitis due to perforated appendix is rarely reported. Our literature review showed that only 16 cases (including this) have been reported with calculated mortality rate of 46.15% (3 cases did not report outcome). Retrocecal appendiceal location is mostly seen to be present. In our patient, the perforated appendix ruptured through peritoneum into retroperitoneal space and drained out into lateral abdominal wall through superior and inferior lumbar triangles (areas of relative weakness) causing extensive necrotizing fasciitis of this region with multiple abscess formation. This case illustrates the importance of early diagnosis of disease, progression, and prompt surgical intervention and why should we be vigilant for clues of a missed silent appendicitis.
CONCLUSIONS:
Although acute appendicitis is one of the most common abdominal pathology, a delay in diagnosis can lead to complications like perforation which can cause life-threatening necrotizing fasciitis. Early recognition, broad-spectrum antibiotics, and timely surgical debridement are crucial. We should consider intra-abdominal pathologies in determining cause of necrotizing fasciitis presenting over abdominal, flank, or hip regions.
Review of literature of all the cases worldwide regarding necrotizing fascitiis due to perforated appendix.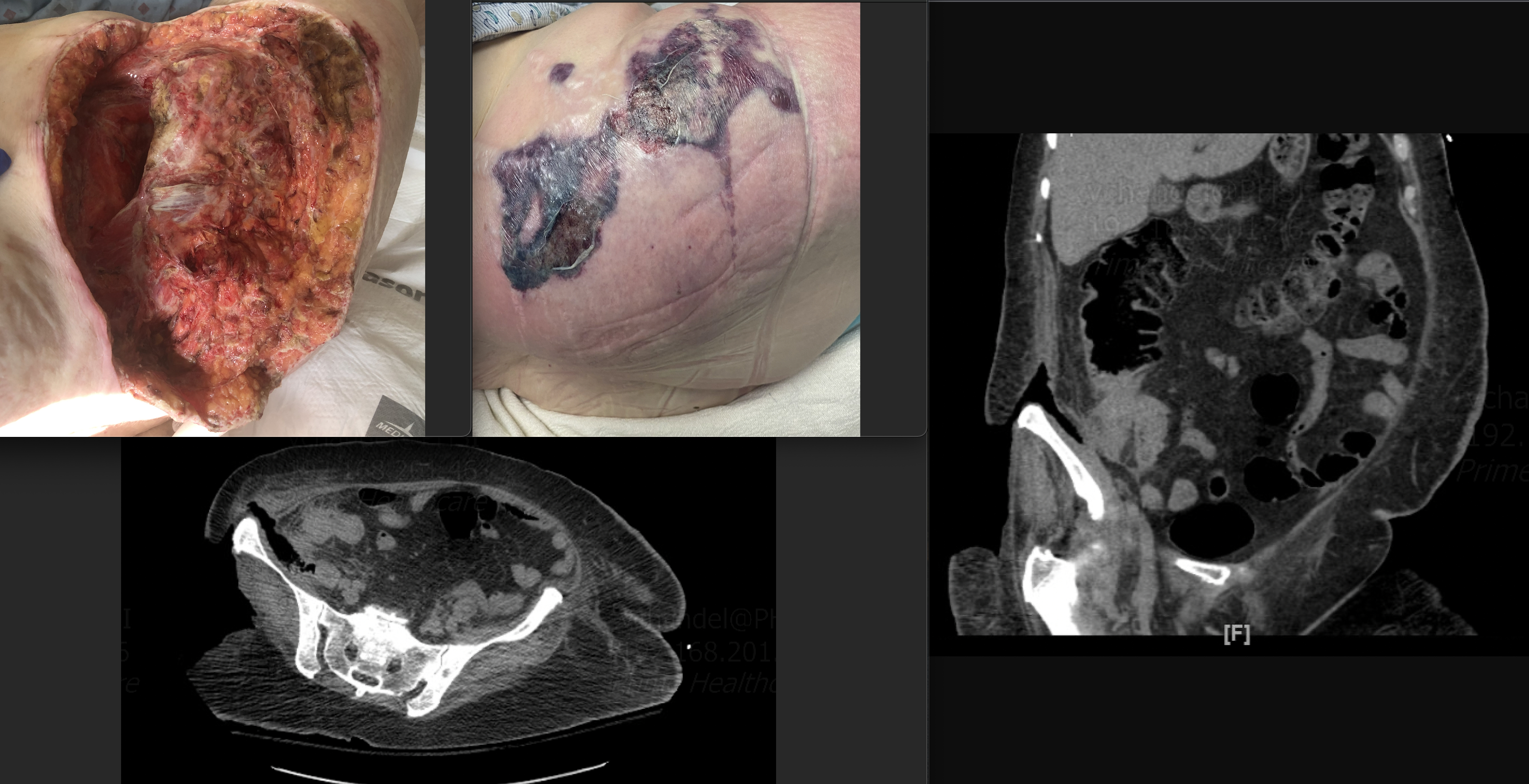
Necrotizing fascitiis from a silent perforated appendix: Upper left shows post operative wound after removing necrotic tissue and abscesses and other one shows wound in healing stages with a wound vac. Lower left shows CT imaging axial view and Right side image shows CT imaging sagittal view of this patient.
Back to 2022 Posters
