TELEMEDICINE USE ASSOCIATED WITH REDUCED NO-SHOW VISITS AMONG GASTROINTESTINAL PATIENTS
Connie Shao*, Chandler McLeod, Andy Hare, Lauren Theiss, Isabel Marques, Burke Smith, Eric L. Wallace, Daniel I. Chu
Surgery, The University of Alabama at Birmingham, Birmingham, AL
Introduction:
Telemedicine has been shown to provide high-quality care with improved convenience for patients. However, whether it has improved access for patients is not known given the digital divide. We therefore aimed to characterize no-show visits (NSV) among a diverse patient population in the Deep South.
Methods:
All patients seen in gastrointestinal medicine (GIM) and surgery (GIS) clinics at a tertiary care academic center in Alabama were reviewed Oct 1, 2020 to Sep 30, 2021. Patient-level (age, race, sex, and insurance) and provider-level (date of service, new patient versus return visit, and department) factors were recorded. In-person, phone, and video-based telemedicine (VBT) visits were analyzed with Chi-square and ANOVA. Factors associated with NSV were analyzed with multivariable logistic regression.
Results:
Of the 33,818 visits, 75% were in-person, 16% via VBT, and 9% were phone calls. In total, 1.4% of visits were NSV. Most were with GIM (66%) and returning (61%). Patients were mostly female (60%), white (66%), and Black (28%). Visits were evenly distributed throughout the week, but least frequently on Fridays (13%). On average, patients were 54 years old (SD=16).
Phone calls were used most by GIS (48% of visits) compared to in-person (32% of visits) and VBT (35% of visits) visits (p<0.001). Male and Black patients were seen in-person (41.5%, 31%) more often than via phone (38%, 28%) or VBT (35%, 26%) (p<0.001, p<0.001). Patients using phone visits were older (58 yr) compared to those seen in-person (54) and via VBT (51), (p<0.001). All phone visits were return visits (100%); only 79% of VBT visits and 53% of in-person visits were return (p<0.001). NSV were more frequent for in-person (1.8%) than phone (0.1%) or VBT (0.0%) visits (p<0.001). Patients using phone visits were more likely to be insured with Medicaid (38%) than those seen in-person (34%) or via VBT (31%) (p<0.001).
On multivariable analysis, NSV were less likely with GS (OR:0.49, 95%CI:0.39-0.62), with older patients (per 1 year OR:0.95, 95%CI:0.94-0.95), mid-week (ref: Mon, Tu OR:0.6, 95%CI:0.45-0.8, Wed OR:0.67, 95%CI:0.5-0.91, Th OR:0.59, 95%CI:0.43-0.8), and with VBT (OR:0.02, 95%CI:0-0.06) or phone calls (OR:0.06, 95%CI:0.02-0.18). Black compared to white race (OR:1.53, 95%CI:1.25-1.87) was associated with NSV. NSV were independent of payor, sex, or time during the study period.
Conclusion:
Phone and video-based telemedicine are significantly associated with reduced NSV. New patient visits are most frequently in-person but converting more return visits to telemedicine can reduce NSV. The disproportionate rate of NSV for Black patients highlights an important gap in access that must be addressed. NSV can be reduced by increasing telemedicine access and uptake through education and culturally appropriate care.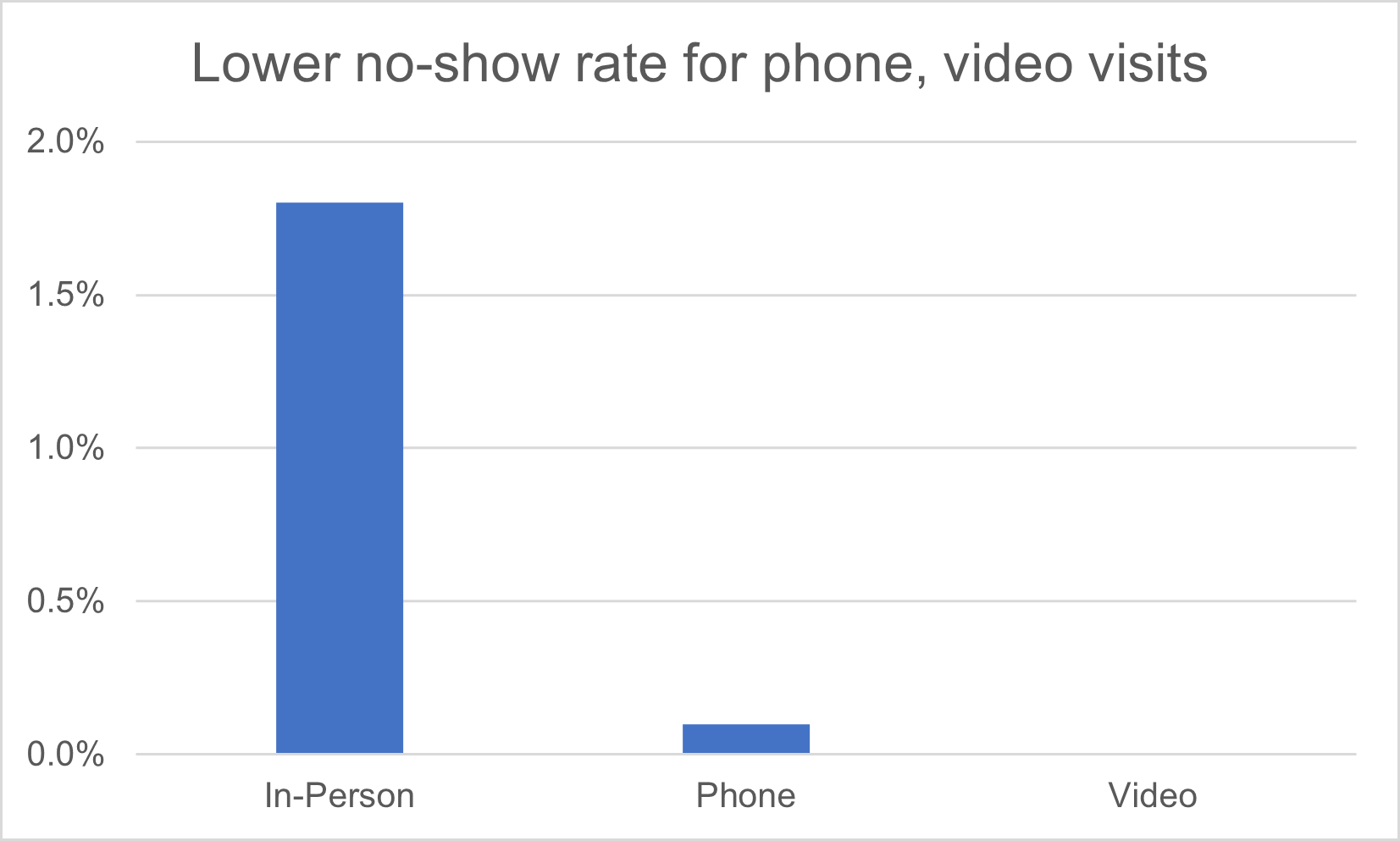
Back to 2022 Abstracts
