OUTCOMES OF PATIENTS WITH ISCHEMIC COLITIS PRESENTING WITH SEVERE HEMATOCHEZIA TREATED MEDICALLY OR WITH SURGERY
Usah Khrucharoen1,2,3, Thongsak Wongpongsalee1,4, Dennis M. Jensen1,2,3, Peerapol Wangrattanapranee*1,3,5, Rome Jutabha1,5, Mary Ellen Jensen1,2,3
1CURE Digestive Diseases Research Center, Los Angeles, CA; 2University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA; 3VA Greater Los Angeles Healthcare System, Los Angeles, CA; 4Mahidol University Faculty of Medicine Siriraj Hospital, Bangkok, Thailand; 5University of Southern California Keck School of Medicine, Los Angeles, CA
Background and aims: Ischemic colitis (IC) is a common cause of severe lower gastrointestinal bleeding especially in patients with multiple comorbidities. Comparisons of outcomes of IC patients presenting with severe hematochezia and treated medically or surgically have not been reported. This study aimed to 1) compare short- and long-term outcomes of hospitalized IC patients presenting with severe hematochezia who were treated with medical management or colectomy and 2) compare clinical outcomes in those who had inpatient vs. outpatient start of hematochezia.
Methods: This is a retrospective study of prospectively collected data for IC patients hospitalized for severe hematochezia from UCLA and VA Medical Centers from 1994-2020. A diagnosis of IC was made during urgent colonoscopy and confirmed histologically. Outcomes were compared for the three groups of patients according to their final treatments and between the two groups according to inpatient vs. outpatient start of hematochezia.
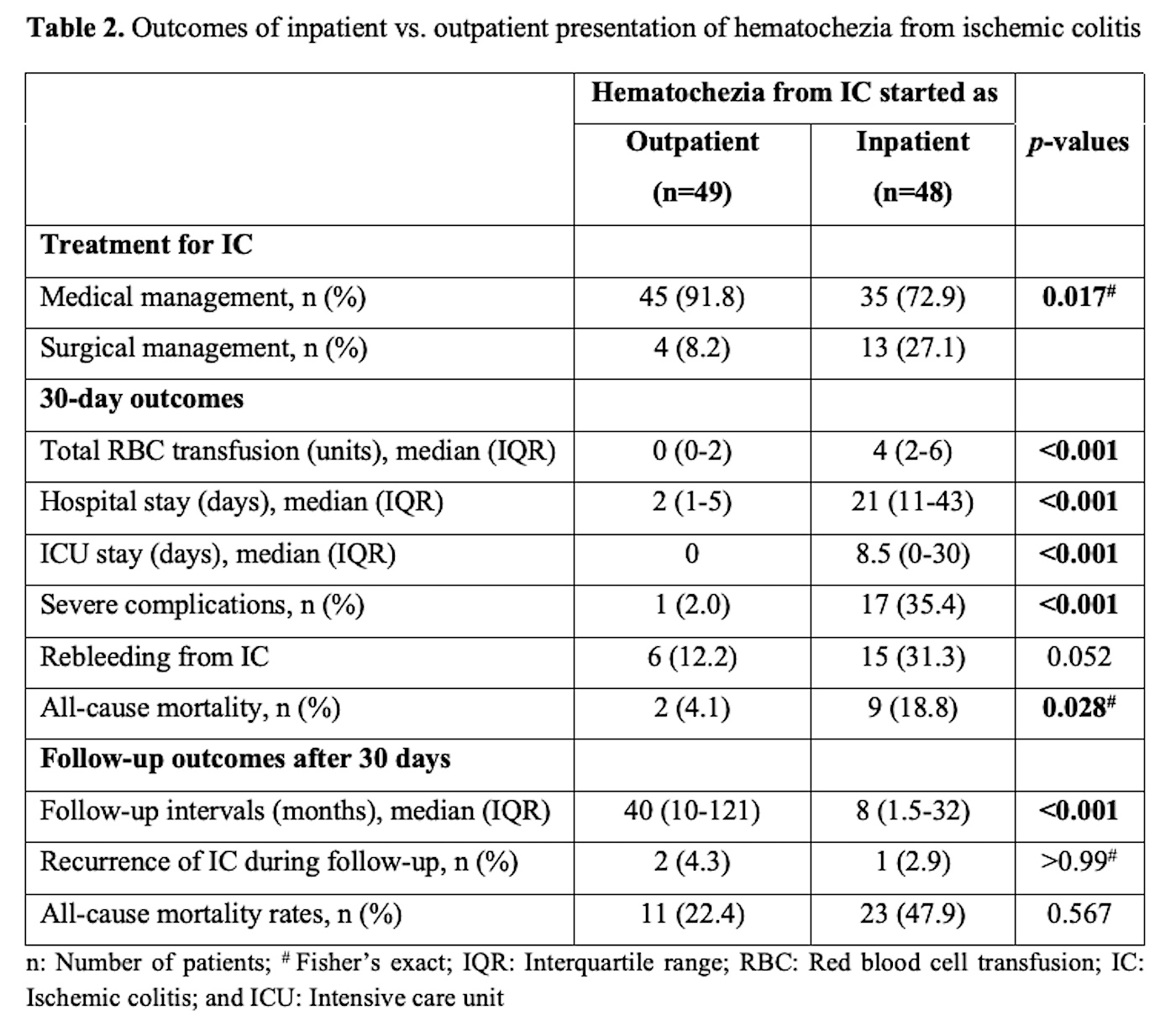
Results: 97 patients with IC were included in this report. All patients initially received medical management for IC. 72 (74.2%) had no further bleeding and clinically improved (Group A). 25 (25.7%) had further bleeding and/or complication indicating the need for surgery. Of these, 17 (17.5%) had colon resection (Group B) and 8 (8.2%) did not have colon resection and received medical treatment due to their poor surgical candidacy (Group C). Demographics were not different for the three groups. However, patients in groups B and C had significantly higher comorbidity scores and received more red blood cell (RBC) transfusions [A vs. B vs. C, median (IQR): 1 (0-4) vs. 5 (3-10) vs. 4.5 (3-6.5) units, p <0.001]; significantly longer hospital and ICU stays; higher severe complication rates (5.6% vs. 35.3% vs. 100%); and higher 30-day all-cause mortality rates (0% vs. 23.5% vs. 87.5%). See Table 1. Patients with hematochezia started as an inpatient (e.g. during hospitalization from other medical conditions) had higher comorbidity scores than those with hematochezia starting as an outpatient. Inpatient hematochezia patients received significantly more units of RBC's, had longer hospital and ICU stays, and had higher rates of severe complications and all-cause 30-day mortality. See Table 2.
Conclusions: The majority of IC patients presenting with severe hematochezia were successfully treated with medical management. Patients who had indications for surgery but were poor surgical candidates and were treated medically had the highest rates of severe complications and 30-day mortality. Patients who had colon resection and those who were poor surgical candidates had worse outcomes than those receiving medical treatment alone. Patients with inpatient start of hematochezia from IC had significantly worse 30-day outcomes than those with hematochezia starting as an outpatient.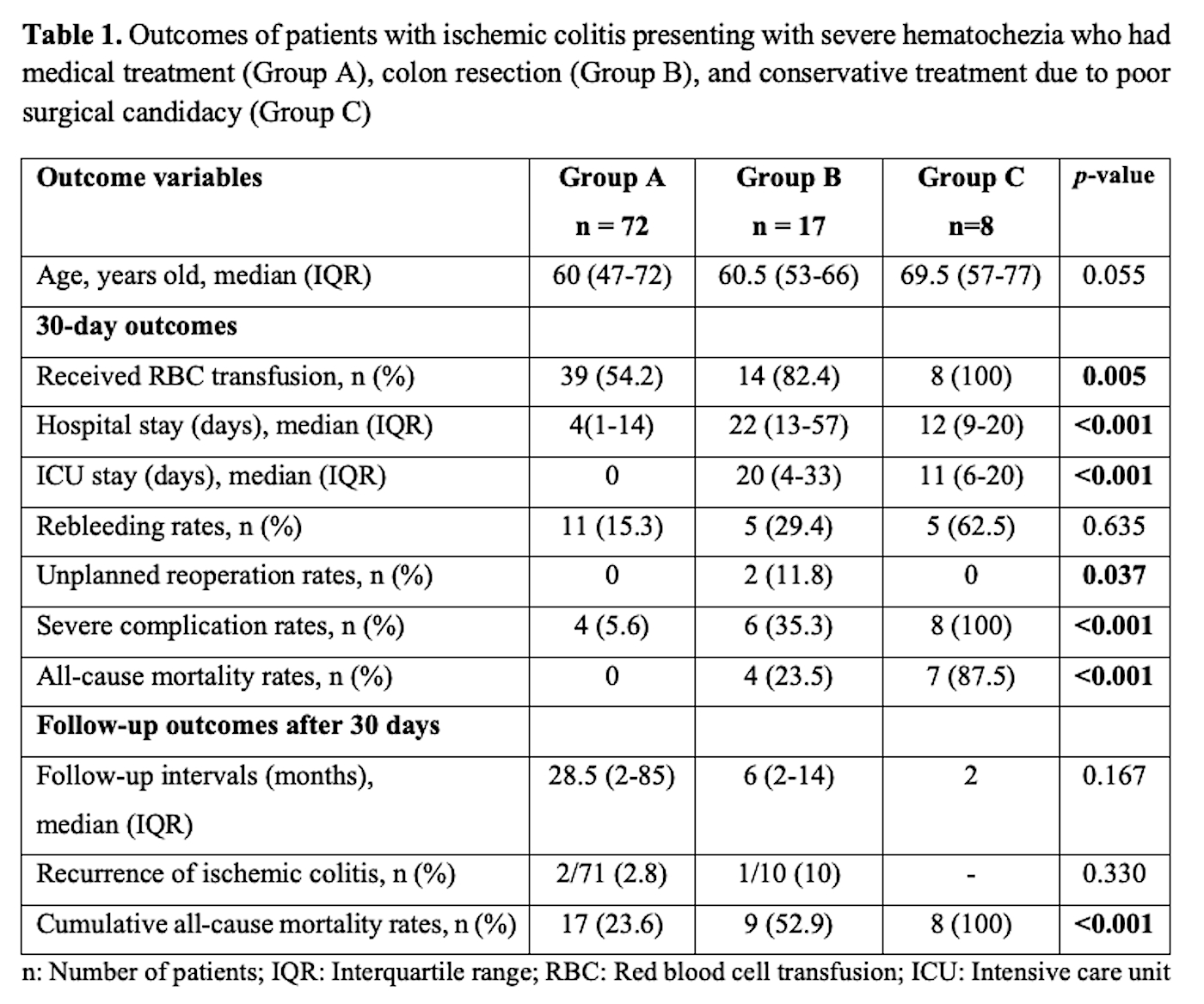
Back to 2022 Posters
