SPONTANEOUS CECAL PERFORATION IN COVID-19 - AN UNCOMMON MANIFESTATION
Vishal Chandel*1, Ryosuke Misawa2, Imran Khokhar1, Phillip Zacco3, Muthukumar Muthusamy3, Rafael Fazylov3
1Suburban Community Hospital, East Norriton, PA; 2Westchester Medical Center, Valhalla, NY; 3Philadelphia College of Osteopathic Medicine - Georgia Campus, Suwanee, GA
BACKGROUND:
Gastrointestinal (GI) manifestations are the most frequently reported extra-pulmonary symptoms of COVID-19 infection with a prevalence of 10%-50%. Most common ones are nausea, vomiting, diarrhea and abdominal pain. GI perforation especially spontaneous colonic perforations are rare in the disease course.
METHODS:
We report the case of a patient with COVID-19 infection, who developed cecal perforation while recovering from COVID pneumonia, necessitating emergent surgical treatment, and the current literature was reviewed.
CASE PRESENTATION:
65-year-old male presented to the hospital with shortness of breath, myalgias and fever. He was admitted to ICU secondary to acute hypoxemic respiratory failure due to COVID 19 pneumonia. He was treated with steroids, tocilizumab and remdesivir. On day-11, he developed severe abdominal pain with worsening leukocytosis. His CXR showed air under diaphragm and abdominal CT showed large pneumoperitoneum, suggestive of a perforated viscus. He underwent emergent laparotomy and was found to have non-obstructive cecal perforation. A colonic de-tension and right colectomy with ileo-transverse anastomosis was performed and he was successfully discharged later. The tissue pathology showed distended colon, active colitis, transmural granulocytic inflammation, micro-abscesses, and ulceration suggestive of bowel perforation.
DISCUSSIONS:
ACE2 protein, a cell receptor for SARS-CoV-2, has been found in glandular cells of gastrointestinal epithelia. Direct viral infection, small vessel thrombosis, or nonocclusive mesenteric ischemia are some possible explanations for the spectrum of bowel findings. SARS-CoV-2 can have direct inflammatory effect on vascular endothelium too. Use of steroids, tocilizumab and systemic coagulopathy seen in severe COVID-19 infection also contributes to these manifestations. In our patient, an acute over-distension of colon, without mechanical distal obstruction, in the setting of COVID-19 infection & tocilizumab led to cecal perforation. Our literature review confirmed only 33 case-reports or series of bowel perforation (either as presenting symptom or during hospital course) in the setting of COVID-19 infection have been reported, with combined 28.5% mortality rate and 5 studies not reporting the outcome. Considering the worldwide incidence of this pandemic, it is a rare complication.
CONCLUSIONS:
GI perforation is a rare but dangerous complication of COVID19. Treatment with interleukin-6 inhibitors or steroids is often associated in most cases. As we are gaining more knowledge about clinical spectrum of this novel disease, we are learning more about its possible rare expression, associations, and complications. Our case underlines the need to be vigilant for severe GI symptoms in setting of COVID-19 infection to enrich our understanding of this pandemic and as a result improve patients' outcome.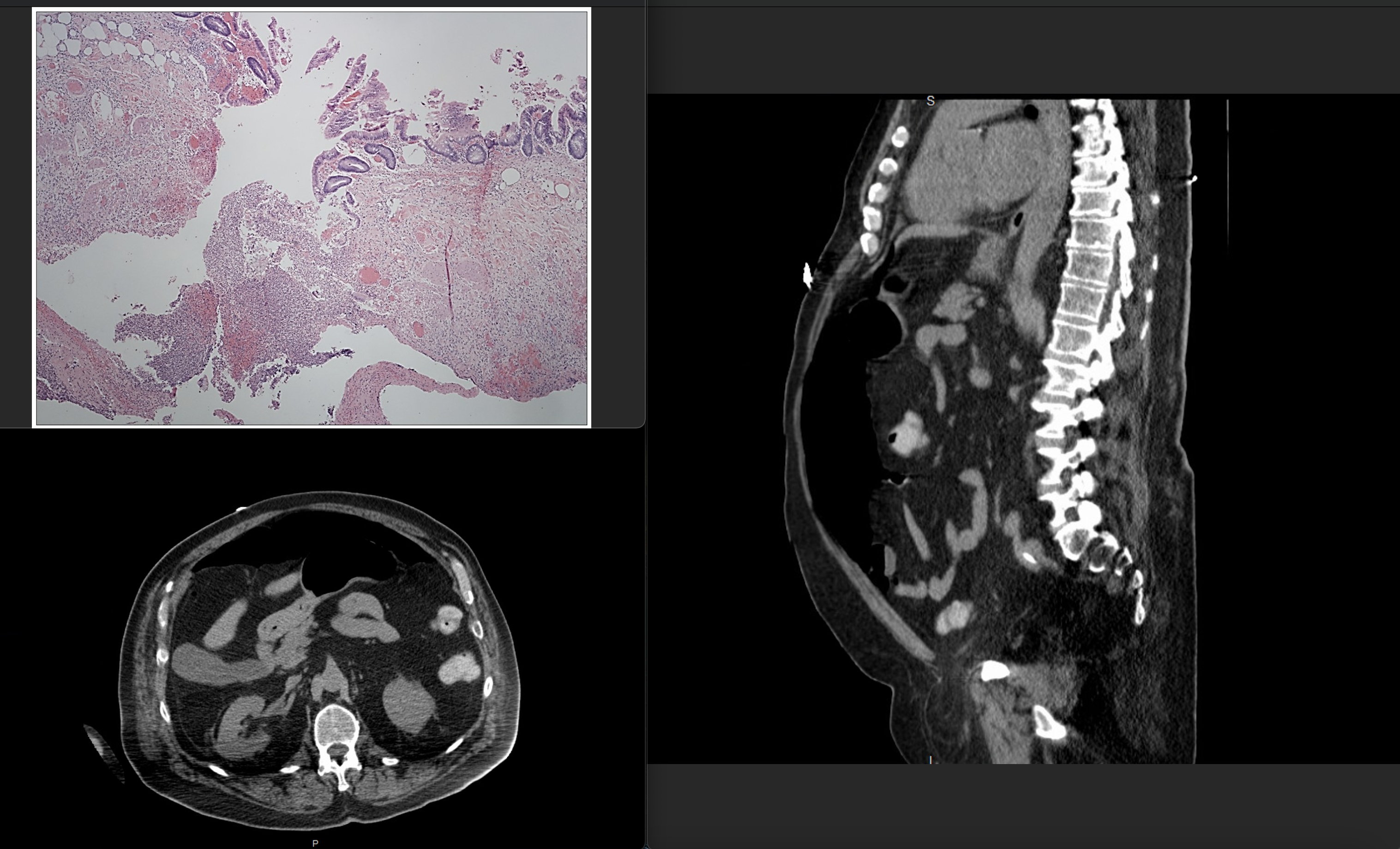
CT imaging showing cecal perforation in axial and sagittal views, along with histological view of the site of perforation.
Review of literature of all worldwide cases of gastrointestinal perforation in association with COVID-19.
Back to 2022 Posters
