DISTAL VERSUS PROXIMAL MICROSCOPIC MARGIN POSITIVITY FOLLOWING ILEOCOLIC RESECTION FOR CROHN'S DISEASE
Adam Truong*, Jino Chough, Karen Zaghiyan, Phillip Fleshner
Cedars-Sinai Medical Center, Los Angeles, CA
Background: Following ileocolic resection for Crohn's disease (CD), active microscopic disease at the resection margin has been associated with recurrence, though few studies compare risk factors for margin positivity.
Aim: We aim to characterize the incidence and impact of distal and/or proximal margin positivity.
Methods: A prospective inflammatory bowel disease registry at a tertiary-referral center was queried for CD patients with positive microscopic margin disease following ileocolic resection (ICR). Intestinal transection was performed in macroscopically and palpably normal bowel. Margins were analyzed by IBD-specialized pathologists blinded to detailed clinical data. Microscopic disease positivity was measured at both proximal and distal resection margins and defined by acute inflammation or crypt distortion. Disease recurrence was defined by endoscopic, radiologic, or clinical evidence of Crohn's-related inflammation, structuring, abscess, or fistula.
Results: Over an 18-year period ending in 2020, we analyzed 469 consecutive patients, of which 60 (13%) patients had a positive microscopic margin following ICR (Table 1). Thirty-eight patients (63%) had a positive proximal margin, 11 (18%) had a positive distal margin, and 11 (18%) had both a positive proximal and distal margin. The median age was 29 (21-46) years and included 31 (52%) females. Most had never smoked (70%) or had quit smoking (22%). Use of preoperative immunomodulators (n=55, 92%) and/or infliximab (n=38, 64%) was common. Most surgeries were the patient's index operation (58%), of which the majority were done laparoscopically (61%) and median resection length was 24 (17-35) cm. Those with double margin positivity were older compared to those with a positive distal margin (40 years [30-57] vs 24 [18-36], p=0.04) and a higher rate of preoperative infliximab use was seen in those with proximal margin positivity compared to those with distal or double margin positivity (76% vs 36% vs 55% respectively, p=0.045). The 60 patient cohort had a median follow-up length of 12 (IQR 5-49) months. Recurrence rates were 82%, 89%, and 90% for those with proximal, distal, and both margin positivity, respectively. Median recurrence-free survival times were similar as well, with no correlation found between specific margins and recurrence (Figure 1; p=0.87).
Limitations: This is a retrospective study. Pathologic details of the positive margins were unavailable.
Discussion/Conclusions: In this largest, single-center prospective series of CD patients undergoing ileocolic resection, we characterize clinical factors associated with distal, proximal, and double margin positivity. Patients with positive proximal margins had a higher rate of preoperative infliximab use and those with double margin positivity were older. No association between any margin positivity and disease recurrence was observed.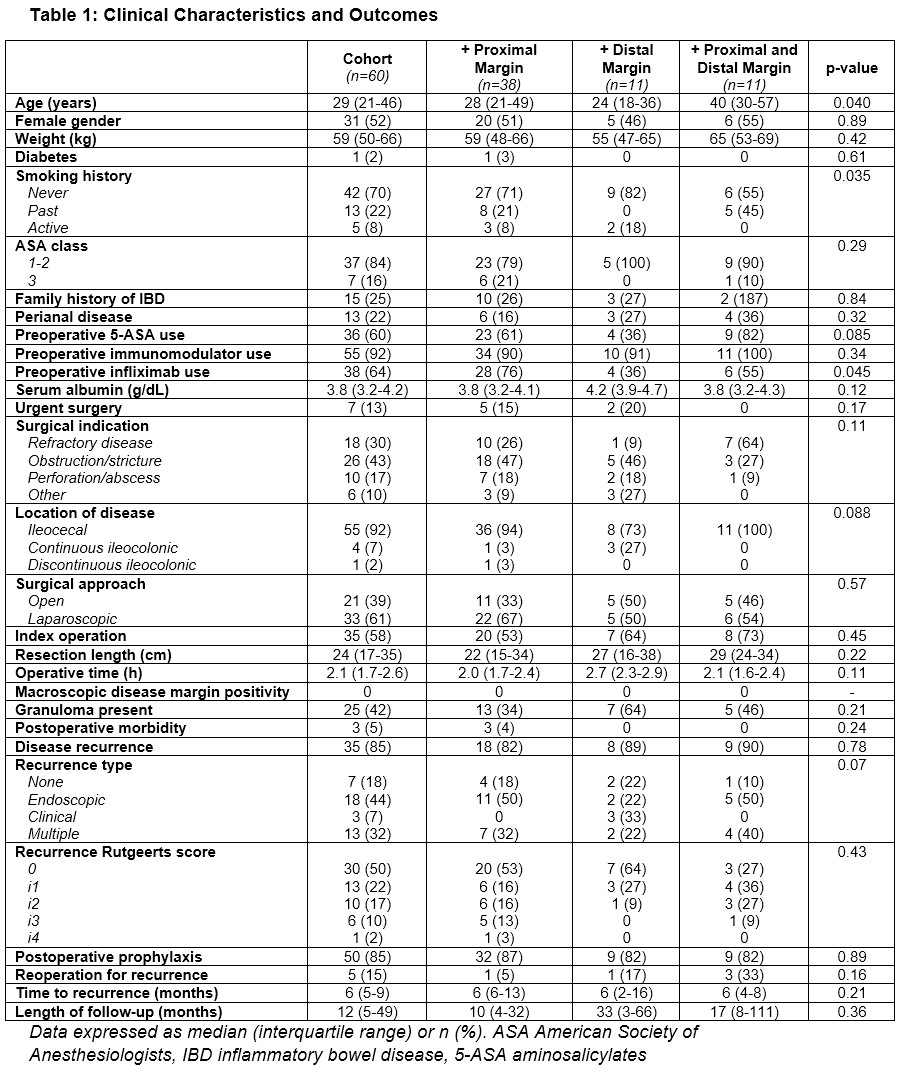
Table 1: Clinical Characteristics and Outcomes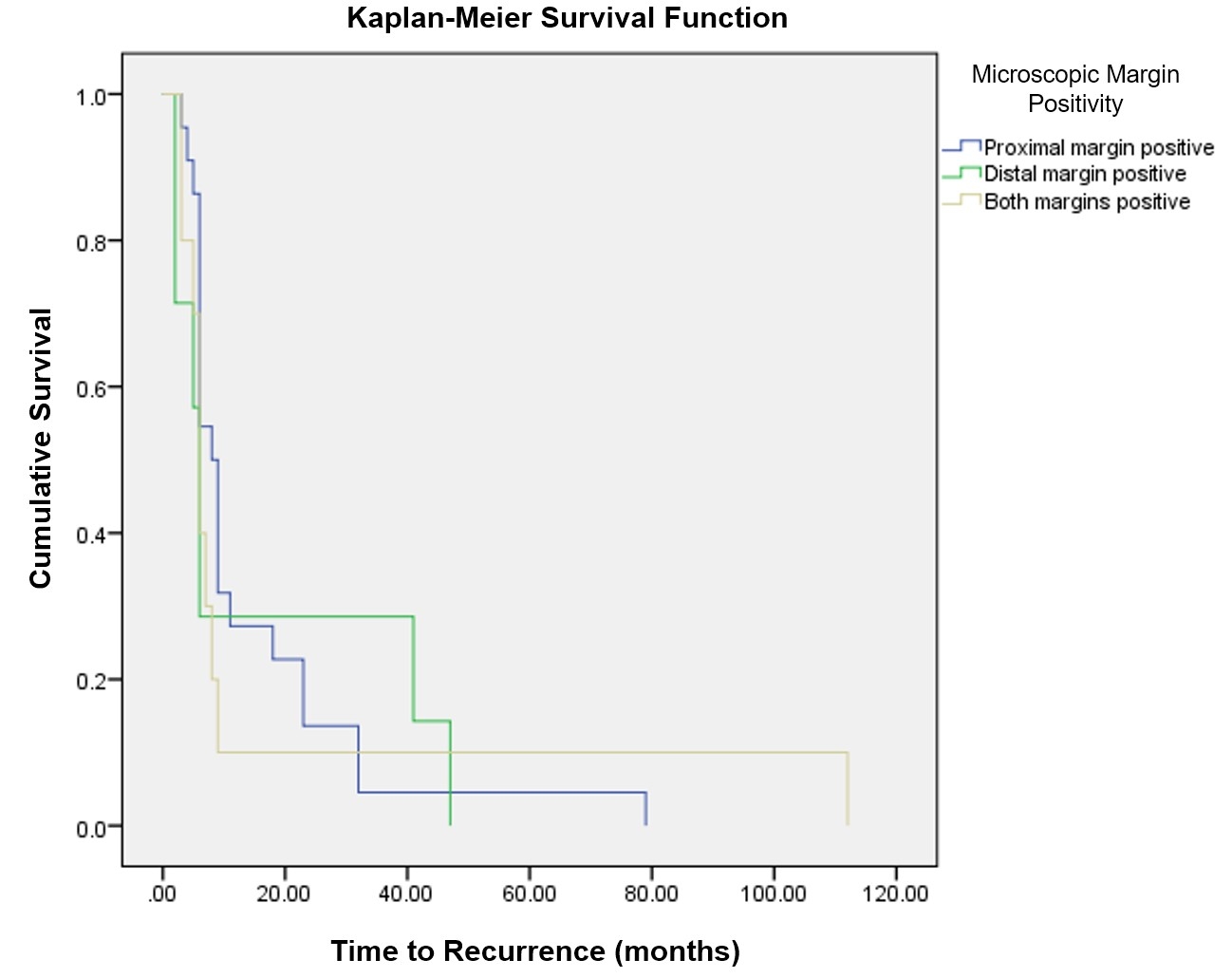
Figure 1: Kaplan-Meier analysis comparing recurrence-free survival between margin-positive groups. Log-rank p=0.87
Back to 2022 Abstracts
