INTRADUCTAL TUBULOPAPILLARY NEOPLASM (ITPN) OF THE PANCREAS WITH MULTIFOCAL INVASION: A CASE REPORT AND REVIEW OF THE LITERATURE
Mohsin E. Jawed*, Carlos Soriano, Michael Wayne, Cathy Fan, Michael Zenilman
Surgery, NewYork-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Intraductal tubulopapillary neoplasm (ITPN) comprises a unique premalignant lesion of the pancreatic epithelium, characterized by high-grade dysplasia and ductal differentiation, and without an overt production of mucin. Arriving at a definitive radiographic and histopathologic diagnosis of this extremely rare entity remains a challenge, as does ascertaining its prognosis relative to similar intraductal neoplasms. Presented in this report is a case of high grade ITPN with multifocal invasion identified after pancreaticoduodenectomy, as well as a literature review aimed at characterizing the identification, features, and clinical significance of ITPN.
Methods/Results: The case is of a 76-year-old female who presented with four weeks of abdominal pain, nausea, and vomiting. She was evaluated with abdominal computed tomography and magnetic resonance imaging, which identified a pancreatic head mass. Endoscopic ultrasound and fine needle aspiration cytology of the lesion yielded adenocarcinoma. There was no evidence of metastatic disease at the time of evaluation. Surgical resection of the specimen was performed (Figure 1), and the diagnosis of ITPN with multifocal invasion was made on histology (Figure 2), with negative surgical margins at resection.
Discussion/Conclusions: ITPN represents a unique lesion of the pancreas that is still poorly defined, accounting for <1% of all pancreatic exocrine neoplasms, and 3% of intraductal neoplasms. It is closely related to the intraductal papillary mucinous neoplasm (IPMN), though distinct due to its tubulopapillary growth pattern and lack of epithelial mucin production. While histology remains the current standard for diagnosis, multiple reports suggest potentially distinguishable features on fine needle aspiration cytology and/or imaging. Preliminary follow-up data from patients with ITPN suggests an overall favorable survival of 100% at 5 years without invasion, and 71% with any component of invasion. This is compared to traditional pancreatic ductal adenocarcinoma, which portends a 5-year survival of 4.2% across all stages. Further investigation is needed to precisely characterize long-term implications on prognosis and survival of patients with this form of pancreatic cancer.
Figure 1. Axial view of CT shows a pancreatic head mass and upstream pancreatic duct dilation with partial encasement of the portal vein.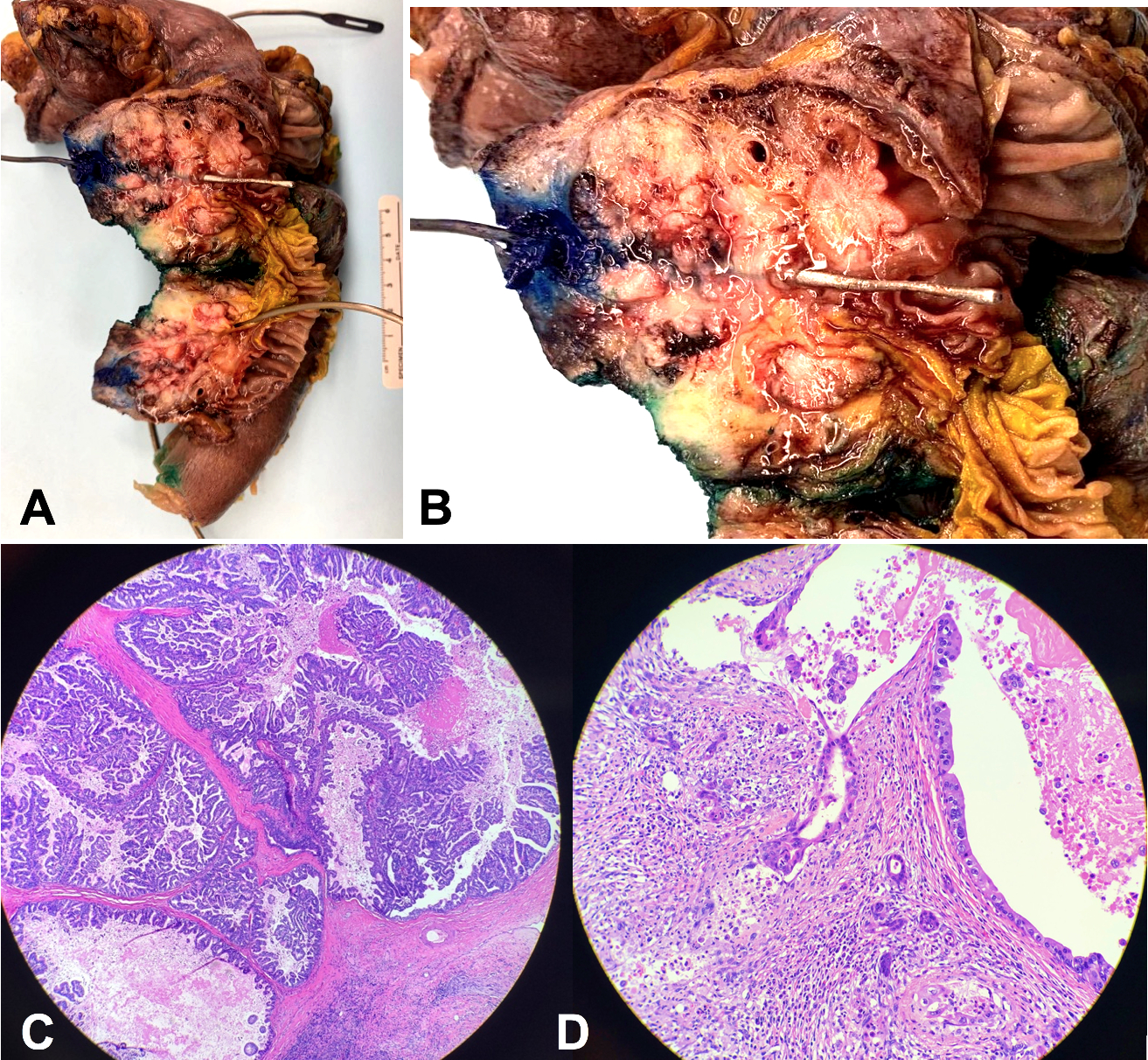
Figure 2. A-B, gross pathology of the resected specimen revealing a poorly defined, pink-grey papillary and indurated tumor at the pancreatic head. C-D, hematoxylin and eosin staining of cross-section through specimen yields a high grade, irregular tubulopapillary growth pattern with multifocal microinvasion up to 1cm. All margins were found to be negative for carcinoma.
Back to 2022 Posters
