SAFETY AND OUTCOMES OF REPEATED LIVER RESECTION FOR COLORECTAL LIVER METASTASES: A REVIEW OF 23 YEARS OF HEPATECTOMY DATA
Allison N. Martin*1, Harufumi Maki1,2, Elsa M. Arvide1, Whitney L. Dewhurst1, Teresa L. Phan1, Timothy E. Newhook1, Hop Tran Cao1, Yun Shin Chun1, Ching-Wei D. Tzeng1, Jean-Nicolas Vauthey1
1Surgical Oncology, The University of Texas MD Anderson Cancer Center Division of Surgery, Houston, TX; 2Tokyo Daigaku Daigakuin Igakukei Kenkyuka Igakubu, Bunkyo-ku, Tokyo, Japan
Background: Rates of liver resections for recurrent colorectal liver metastases have become increasingly common at high-volume hepatobiliary centers. We sought to compare safety and outcomes for patients undergoing single hepatectomy compared to patients undergoing repeated liver resections.
Methods: Twenty-three years of consecutive hepatectomies for colorectal liver metastases (CRLM) from a single institutional database (1/1998 through 5/2021) were collected and characterized, including clinicopathologic characteristics, perioperative factors, somatic gene mutations, and 90-day outcomes, such as Clavien-Dindo (C-D) complications, including liver-specific complications and surgical site infections (SSIs). Patients undergoing combined procedures and planned 2-stage hepatectomy were excluded. Patients undergoing single resection were compared to those undergoing repeated resection using a propensity score matching (PSM) approach, stratified by eight preoperative variables.
Results: A total of 1,948 patients meeting criteria underwent primary liver resection for CRLM during the study period. Among those patients, 1,661 (85.3%) underwent a single, primary ("initial") hepatectomy and 287 (14.7%) underwent repeated hepatectomy. Of patients undergoing repeated hepatectomy, 36 (12.5%) underwent ?3 repeated resections. Patients undergoing repeated hepatectomy had similar age, sex, median operative time, estimated blood loss and transfusion rates to patients undergoing initial hepatectomy (all p>0.05). Repeated hepatectomy patients were more likely to have a rectal cancer primary (22% vs. 5.6%, p<0.001) and receive portal vein embolization (10.3% vs. 6.2%, p=0.02); initial hepatectomy patients were more likely to receive pre-resection chemotherapy (55.5% vs. 28.7%, p<0.001) and undergo major hepatectomy (49.2% vs. 23.6%, p<0.001). Rates of RAS mutations were higher in the initial hepatectomy group (55% vs 43%, p=0.02). Propensity score matching (PSM) was performed to account for differences in perioperative characteristics between initial and repeated hepatectomies. After successful matching, PSM groups of 70 patients each were produced. Rates of grade 3 or higher C-D complications, bile leakage and surgical site infection (SSI)/wound complications were higher, and operative time was longer in the repeated group compared to the initial group (see Table 1). Length of stay did not differ between groups (p>0.05).
Conclusions: Repeated hepatectomy is a technically demanding procedure; repeated surgery should be considered for a carefully selected patient population. Surgeons should be aware of the higher risk of 90-day postoperative bile leak and SSI in patients undergoing repeated hepatectomy, even for repeated hepatectomy patients with an initially routine postoperative course.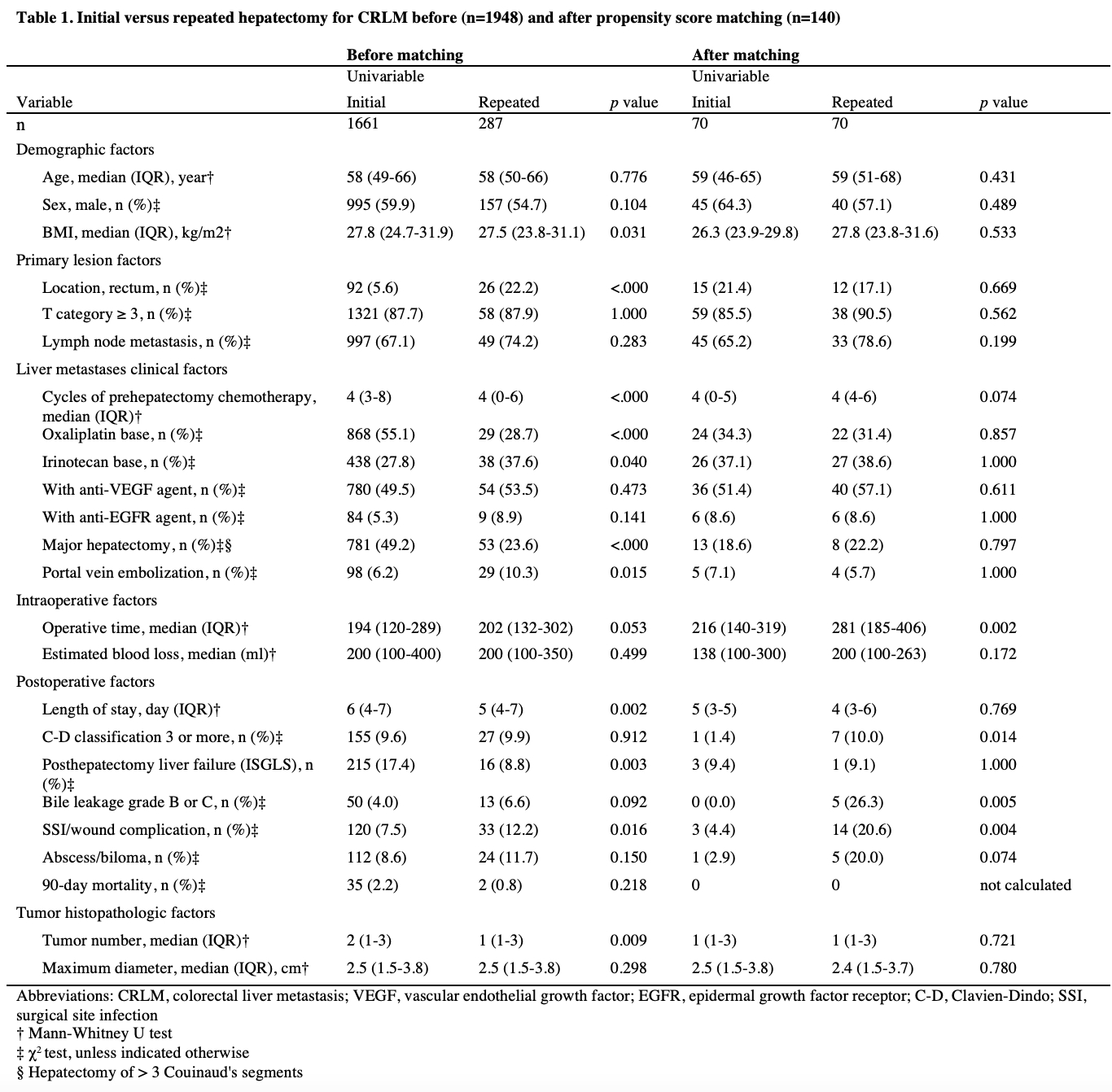
Back to 2022 Abstracts
