CAUDAL-TO-CRANIAL BUT NOT MEDIAL-TO-LATERAL APPROACH IN LAPAROSCOPIC RIGHT COLECTOMY HARVESTS MALIGNANT D3 STATION LYMPH NODES: A CROSS- SECTIONAL STUDY
Beishi Zheng*1, Yichen Wang2, Bing Chen3, Xin Zheng4, Liaonan Zou5
1Internal Medicine, Woodhull Medical Center, Brooklyn, NY; 2Trinity Health Of New England Medical Group Agawam Office Silver Street, Agawam, MA; 3NYU Langone Health, New York, NY; 4Loma Linda University Adventist Health Sciences Center, Loma Linda, CA; 5The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou, Guangdong, China
BACKGROUND: Currently, the medial-to-lateral approach is widely used in laparoscopic right colectomy. However, this approach is unable to completely dissect the lymph nodes posterior to the superior mesenteric vessels. Our aim is to discuss the possibility of cancer cell metastases to these lymph nodes, as well as whether or not it is necessary and if so, how to dissect these lymph nodes by using the caudal-to-cranial approach.
METHODS: A total of 156 consecutive patients (from Jan 2015 to June 2020) prospectively selected with confirmed right colon cancer underwent a curative laparoscopic right colectomy were randomly divided into two groups, the caudal-to-cranial approach group (CtC group) and the medial-to-lateral approach group (MtL group). All cases received preoperative carbon nanoparticles injections around the tumor via colonoscopy. Lymph nodes harvested during and after procedure were then analyzed by using a lymph node map. The lymph nodes' numbers, locations and positive rate were recorded and calculated.
RESULTS: The baseline data was not significantly different between these two groups (p> 0.05). The mean operation time and intraoperative blood loss in the CtC group and the MtL groups were 162.9±25.36 mins versus 163.5±29.55 mins and 82.0±19.21ml versus 85.3±24.67ml, respectively, without significant difference (p=0.22 and p=0.37). Compared with the MtL group, there was no significant difference in total postoperative complication rate in the CtC group, 15.4% vs 21.8% (p=0.3035). The mean number of total and positive harvested lymph nodes in these two groups were 19.68±6.56 versus 15±3.93(p=0.035) and 2.57±1.75 versus 1.53±2.75(p=0.23), respectively. However, of these positive lymph nodes, 1.1±4.69 were posterior to the superior mesenteric vessels, with a positive rate of 1.3%.
CONCLUSIONS: There were positive lymph nodes posterior to the superior mesenteric vessels in progressive right colon cancers. It may have some advantages by using the caudal-to-cranial approach to harvest D3 station lymph nodes, especially posterior to the superior mesenteric vessels, the long- term prognosis remains to be determined.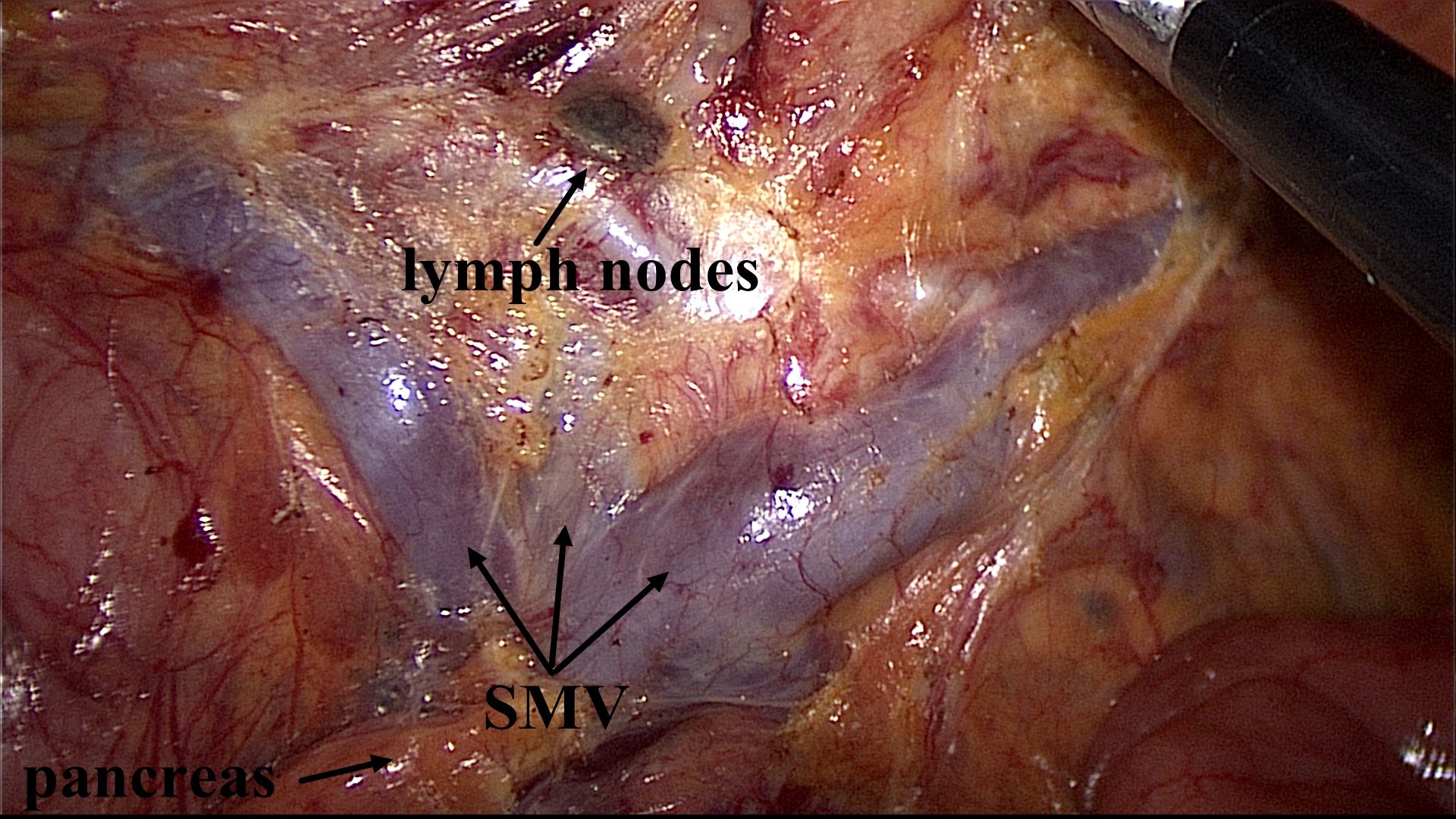
Lymph nodes posterior to the superior mesenteric vessels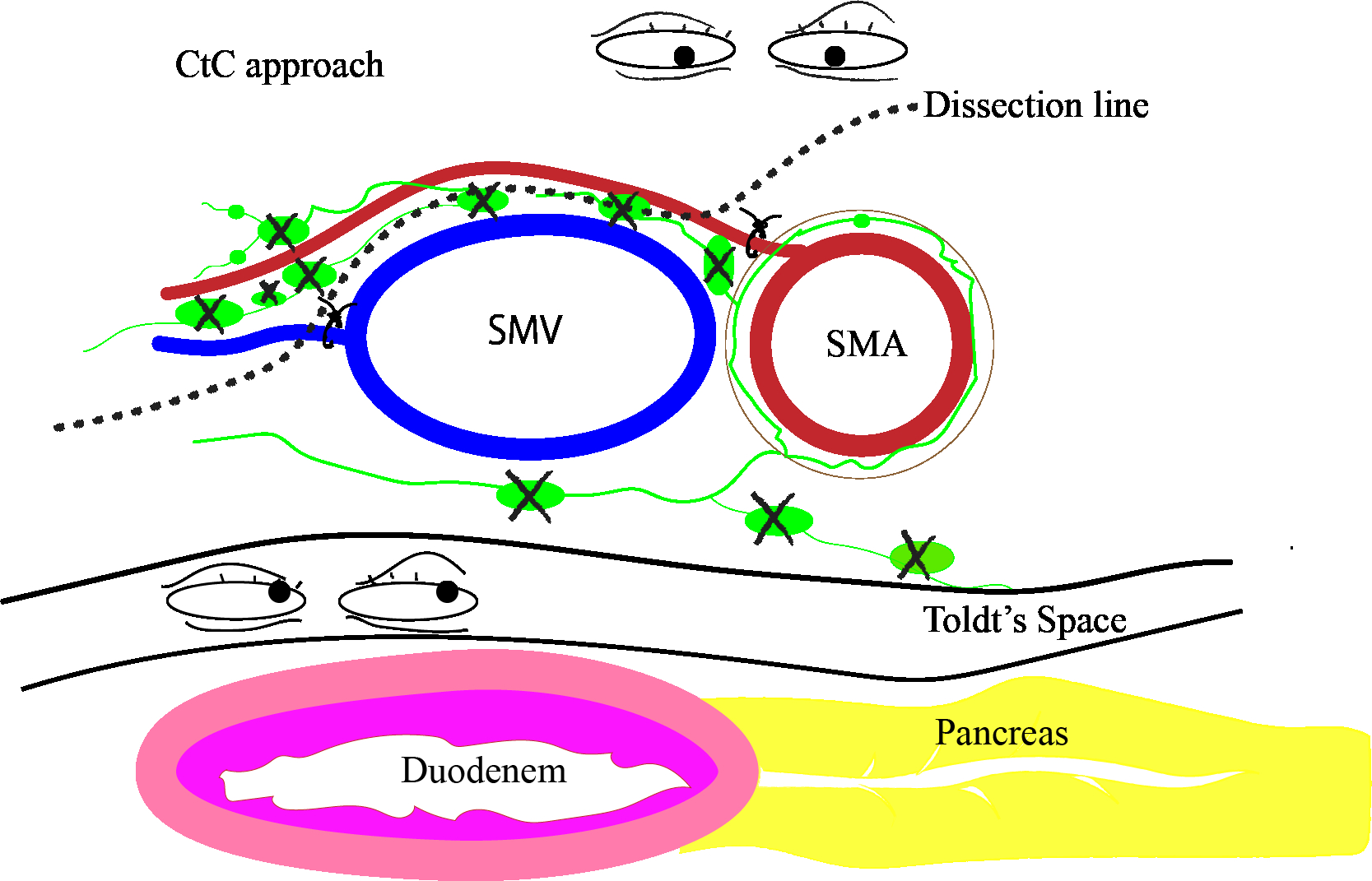
The mechanism of the caudal-to-cranial approach to harvest lymph nodes posterior to the superior mesenteric vessels
Back to 2022 Abstracts
