RESOLUTION OF OBSTRUCTION IN A PATIENT WITH HYPERTROPHIC OBSTRUCTIVE CARDIOMYOPATHY FOLLOWING WEIGHT LOSS SURGERY
Paul Travers*, Victoria Gomez, Mohamad Yamani, Scott A. Lynch, John Stauffer
Internal Medicine, Mayo Clinic's Campus in Florida, Jacksonville, FL
Introduction
Hypertrophic cardiomyopathy (HCM) is a cardiac disease with a known genetic predisposition and variable clinical presentation and illness severity, as well as an association with other conditions, such as obesity. The presence of a significant left ventricular outflow tract obstruction (LVOTO), defining the disease as Hypertrophic Obstructive Cardiomyopathy (HOCM), is associated with worse clinical presentation at the time of diagnosis as well as poorer prognosis. The incidence of obesity among the HCM population has been found to be higher than that of the general population, and obesity has been recently found to predispose to the development of LVOTO, and thus, poor disease progression. However, the relationship between weight loss in patients with HOCM and its effects on LVOTO has not been well studied. We describe a case of a patient with morbid obesity that underwent bariatric surgery for weight loss and experienced resolution of his LVOTO. This case emphasizes the important role of weight loss in the improvement of cardiac diseases, specifically its impact in dramatically improving LVOTO in the setting of HOCM.
Case Presentation
A 65-year-old gentleman with class 3 morbid obesity (BMI 40.3 kg/m2) and HCM presented for a cardiac evaluation prior to bariatric surgery. A preoperative echocardiogram demonstrated HOCM with a peak resting gradient of 12 mmHg that increased with induction via Valsalva maneuver to 81 mmHg (pathologic gradient is defined as ?30 mmHg at rest or with induction maneuvers, and mechanical intervention via septal myectomy is pursued at values ?50 mmHg). During this time, he was symptomatic with exertional dyspnea. He underwent a laparoscopic sleeve gastrectomy with an uneventful postoperative course. Over 9 months, the patient lost a total of 39.2 kg for a BMI of 28.0 kg/m2, for a 31% total body weight loss (%TWL). Followup echocardiography showed resolution of peak resting gradient to 0 mmHg and reduction of inducible gradient with Valsalva maneuver to 6.58 mmHg. Additionally, the patient's exertional dyspnea had resolved. At four years post-op, he had regained 12kg (BMI 31.6 kg/m2), and repeat echocardiography showed a partial return of LVOTO, with a peak resting gradient of 12 mmHg that increased with Valsalva maneuver to 17 mmHg.
Conclusion
While the presentation and disease severity of HOCM is variable, obesity is a modifiable risk factor that is increasingly being associated with worse LVOTO and poorer prognosis. The pathophysiology of this association is incompletely understood, but it is important for the practicing provider to be aware of the serious cardiac diseases and manifestations associated with obesity and metabolic diseases. Future studies should evaluate the benefits of early weight management interventions in patients with obesity-associated HOCM.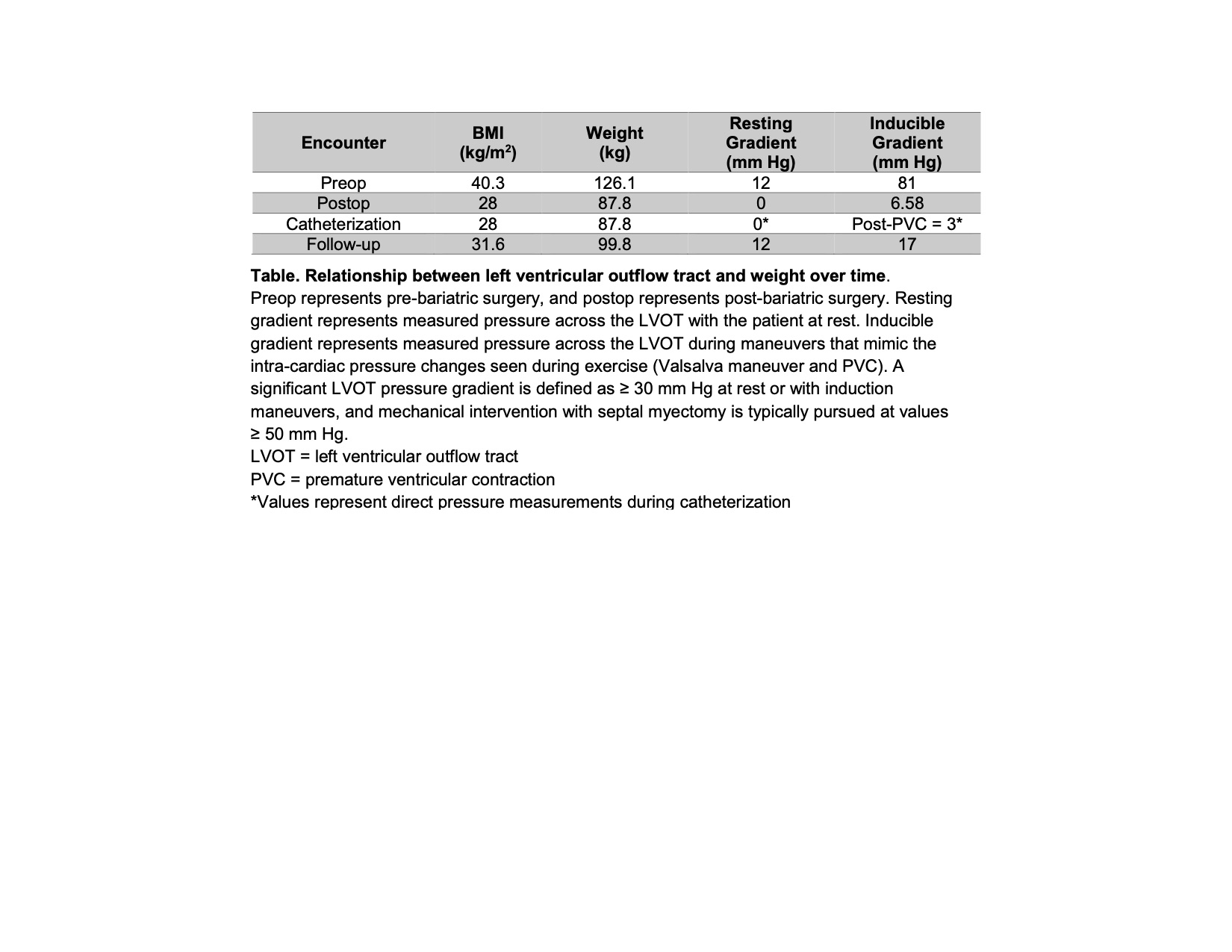
Back to 2022 Posters
