PATIENT ENGAGEMENT TECHNOLOGY (PET) IS ASSOCIATED WITH REDUCED LENGTH-OF-STAYS AFTER COLORECTAL SURGERY EVEN UNDER AN ENHANCED RECOVERY PATHWAY
Lauren Theiss*, Lauren Wood, Isabel Marques, Drew J. Gunnells, Karin M. Hardiman, Jamie A. Cannon, Melanie S. Morris, Gregory D. Kennedy, Daniel I. Chu
University of Alabama at Birmingham (UAB), Birmingham, AL
Background
Patient engagement technologies (PETs) are designed to support the care of patients through a health encounter. In surgery, these technologies guide patients through complex perioperative processes including education, pre-operative preparations and post-operative activities. Limited evidence exists, however, to link PETs with improved surgical outcomes. In this study, we aimed to determine the impact of a PET on surgical outcomes in colorectal surgery in the setting of an Enhanced Recovery Program (ERP).
Methods
Patients undergoing colorectal surgery under an ERP at a single institution were enrolled in a PET (SeamlessMD). Patients received logic-based healthcare reminders, educational content, and surveys pre-operatively, in-hospital, and 30-days after discharge. This PET (2018-2019) group was compared to a pre-PET control group (2017) comprised of patients undergoing colorectal surgery under ERP at the same institution. The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database was queried for patient characteristics and outcomes for both groups. Patients were excluded if they were not included in the ACS-NSQIP database. Primary outcome was length-of-stay (LOS) and secondary outcomes were 30 day readmission, complications, and mortality rates. Adjusted analysis were performed with multivariable regression for outcomes.
Results
A total of 663 patients were included: 514 pre-PET (2017) and 149 PET (2018-2019). Overall median age was 57.4 with an older age in the pre-PET group (58 vs. 55.6, p=0.04). Patient gender, race, functional status, and comorbidities did not significantly vary between the groups. There was no significant difference in 30 day readmission rate, overall complication rate, or mortality rate between the two groups (Figure 1). Median LOS significantly varied between the two groups with median LOS of 3 days for the PET group versus 4 days for the pre-PET group (p=0.04, Figure 2). On adjusted comparison, longer LOS was associated with the pre-PET group (OR 1.04, CI 1.01-1.08, p=0.015).
Conclusion
Colorectal surgery patients using a PET under ERP had an even shorter LOS when compared to pre-PET patients. Use of a PET did not further reduce readmissions or complications. PETs may be useful adjuncts to surgical recovery pathways, but opportunities remain to understand how best to use them.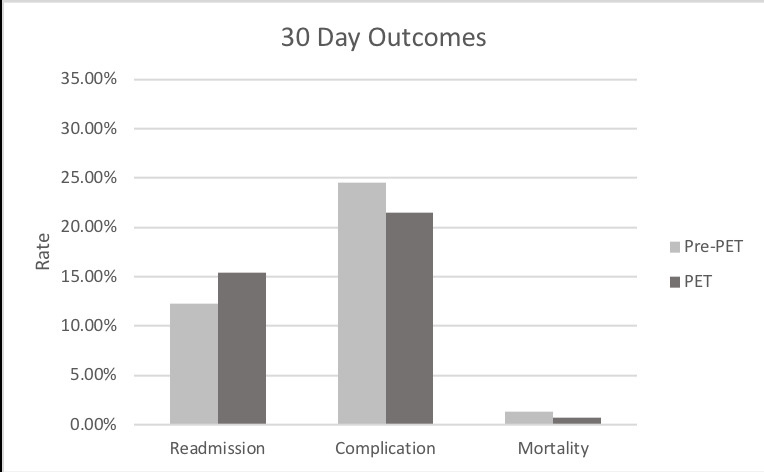
Figure 1.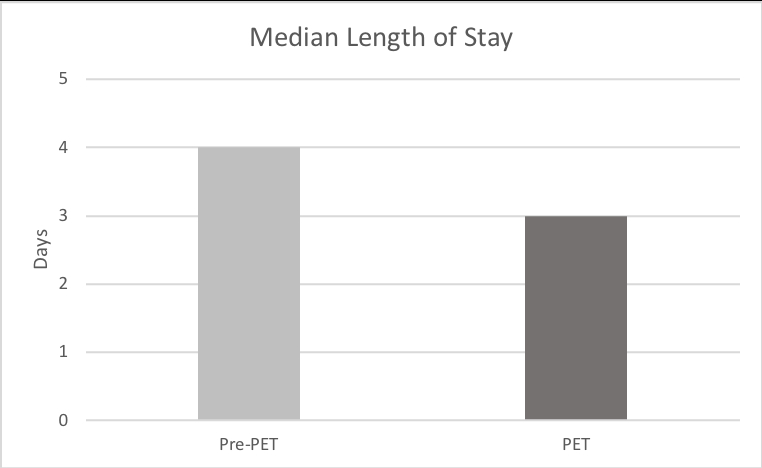
Figure 2.
Back to 2020 Abstracts
