OVERALL VOLUME OF UPPER GASTROINTESTINAL SURGERIES POSITIVELY IMPACTS GASTRIC CANCER OPERATION OUTCOMES AT CENTERS WITH A LOW GASTRECTOMY VOLUME
Susanna W. de Geus*, Krista Hachey, Sing Chau Ng, Michael Cassidy, David McAneny, Jennifer F. Tseng, Teviah Sachs
Boston Medical Center, Boston, MA
Background: The relationship between hospital volume and surgical mortality is well established. However, complete centralization of care is not always feasible, due to geographic constraints, insurance status, or patient preference. The present study investigates how overall upper gastrointestinal surgery volume may influence the outcomes of gastric resection for gastric adenocarcinoma at low-volume centers.
Methods: The National Cancer Database (2004-2014) was queried for patients who underwent gastrectomy for gastric carcinoma. Hospital volume was determined separately for all upper gastrointestinal (esophageal, gastric, duodenal) operations and gastrectomy. Centers were dichotomized as low- and high-volume centers based on the upper quartile. Three study cohort were created: low-volume (LV) centers for both gastrectomies and upper gastrointestinal operations, mixed-volume (MV) centers with low-volume gastrectomy but high-volume upper gastrointestinal operations, and high-volume gastrectomy centers (HV). Multivariable logistic regression analysis with backward selection were performed for various surgical outcomes.
Results: In total, 16,636 patients were identified, 71.2%, 3.7%, and 25.1% patients were treated at LV, MV, and HV, respectively. 30-day mortality was 4.9% in LV, 3.1% in MV, and 2.7% in HV. On multivariable analysis, patients treated at LV showed higher 30-day mortality compared to patients treated at HV (Odds Ratio [OR], 1.65; p<0.001). However, patients treated at MV demonstrated comparable 30-day mortality to HV (OR, 1.10; 0.718). Positive resection margins were found in 14.3%, 10.1%, and 9.4% of patients treated at LV, MV, and HV centers, respectively. Surgery at a LV was significantly predictive for a higher positive margin rate compared to HV (OR, 1.47; p<0.001), but patients at MV demonstrated similar positive margin rates to patients treated at HV (OR, 1.10; p=0.542) on multivariable analysis. Over > 16 lymph nodes were examined in 45.0% of patients treated at LV, 58.3% at MV, and 63.0% at HV. On multivariable analysis, resection of ≤ 15 lymph nodes was significantly more common at LV than HV (OR, 2.12; p<0.001), but comparable at MV and HV (OR, 1.19; p=0.053). Median hospital stay was 8 days at LV, 9 days at MV, and 8 days at HV. Patients treated at LV and HV demonstrated similar length of stay (OR, 0.96; p=0.258), as well as patients who underwent surgery at MV and HV (OR, 1.14; p=0.151).
Conclusion: Gastrectomy outcomes at low-volume centers that have extensive experience with upper gastrointestinal surgery are similar to postoperative outcomes at with a HV. These hospitals provide a model for gastrectomy outcomes to improve quality and access for patients who cannot receive care at HV centers.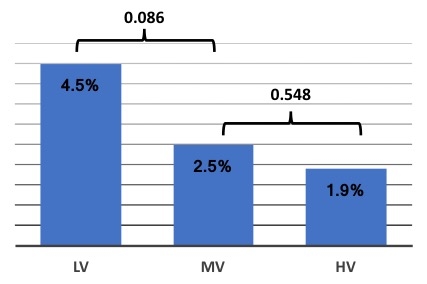
Back to 2020 Abstracts
