DEVELOPMENT OF A NOMOGRAM TO PREDICT INDIVIDUAL BENEFIT ATTAINED FROM ADDITION OF ADJUVANT CHEMOTHERAPY IN THE TREATMENT OF STAGE II COLON CANCER
Clay M. Merritt*1, Shu-Ching Chang2, Gary L. Grunkemeier2, Scott Steele4, Melanie Goldfarb3, Daniel Nelson1
1Surgery, William Beaumont Army Medical Center, El Paso, TX; 2Medical Data Research Center, Providence St. Joseph Health, Portland, OR; 3John Wayne Cancer Institute, Santa Monica, CA; 4Cleveland Clinic, Cleveland, OH
Background: At present, there is inconclusive evidence from randomized controlled trials to define the role of adjuvant chemotherapy (AC) in resected stage II colon cancer. Current guidelines propose consideration of AC for stage II patients with poor prognostic clinicopathologic and molecular features. However, the relative impact of each individual feature or constellation of high-risk features remains undefined. We sought to develop an individualized point-of-care tool to predict the survival benefit attained from the addition of AC in patients with resected curative-intent stage II colon cancer.
Methods: The National Cancer Database was queried for all patients with resected stage II colon cancer from 2004-2015. Twelve clinicopathologic and molecular prognostic factors previously associated with outcomes for colon cancer were compared in patients receiving AC to those undergoing surgery alone in order to construct a nomogram for overall survival (OS): age, sex, Charlson Comorbidity Index, histology, pathological tumor stage, grade, number of nodes examined, margin status, microsatellite instability, carcinoembryonic antigen level, perineural invasion, lymphovascular invasion and adjuvant chemotherapy status. The nomogram was validated for discrimination and calibration using bootstrap-adjusted Harrell’s concordance index (C-index). For estimation at a population level, a prognostic Risk Score was constructed and weighted with beta coefficients estimations in the same model. OS was compared based on quartiles of prognostic risk groups.
Results: Of 132,666 patients with stage II colon cancer, 16.8% received AC and 83.2% had surgery alone as treatment. The calibration curve of the constructed nomogram showed good agreement between predicted and observed median, 3-, 5- and 10-year survival (bootstrap adjusted C-index 0.699, CI: 0.698-0.703). Using the population level Risk Score analysis [median (Q1, Q3); 4.9 (4.6, 5.5)], patients with scores >3.34 demonstrated a significantly decreased risk of death with the addition of AC (Risk Score 3.34-Q1: HR: 0.81, 95% CI: 0.76-0.87, p<0.001; Q1-Q2: HR: 0.78, 95% CI: 0.73-0.82, p<0.001; Q2-Q3: HR: 0.78, 95% CI: 0.74-0.82, p<0.001; >Q3: HR: 0.65, 95% CI: 0.61-0.69, p<0.001). There was no significant survival benefit from AC among patients with low risk scores (Risk Score <3.34: HR: 0.94, 95% CI: 0.80-1.11, p=0.47) (Figures 1A and 1B).
Discussion: A composite weighted nomogram is critical to individualizing the utilization of AC in select high-risk patients. This nomogram provides individualized prognostication and estimation of potential benefit attained from AC based on the individual’s constellation of high-risk features. This may better inform treatment decisions as well as aid future trial design.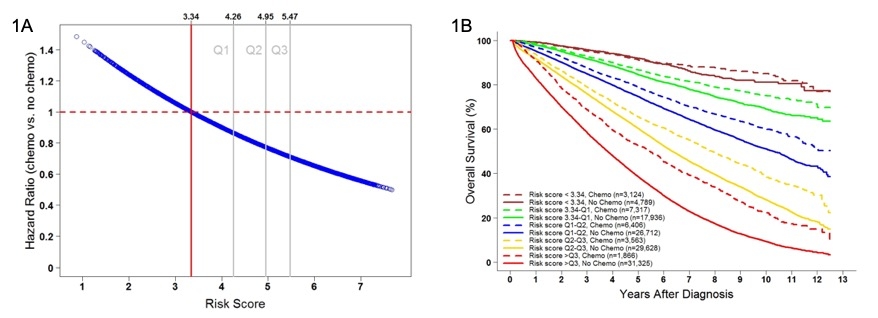
Figure 1. A) Plot of hazard ratio (for mortality) with chemo (ref: no chemo) versus prognostic Risk Score. B) OS compared based on quartiles of prognostic risk groups.
Back to 2020 Abstracts
