|
Back to 2018 Posters
OUTCOME AND COST ANALYSIS OF HOSPITAL TRANSFERRED PATIENTS UNDERGOING EMERGENT COLORECTAL SURGERY
Xian Hua Gao*1,2, Hanumant Chouhan1, Emre Gorgun1, Luca Stocchi1, Gokhan Ozuner3
1Colorectal Surgery, Cleveland Clinic, Shaker Heights, OH; 2Colorectal Surgery, Changhai Hospital, Shanghai, Shanghai, China; 3Department of Colon and Rectal Surgery, Mercy Health, Lorain, OH
BACKGROUND: The effect of inter-hospital transfer on patient outcomes varies in different specialties. There is no single institution study that examines the impact of patient transfer on emergent colorectal surgical procedures.
OBJECTIVE: Our aim was to compare the cost and surgical outcomes of emergent colorectal procedures between inter-hospital transferred patients vs. patients directly admitted to a single institution.
DESIGN: A prospectively maintained database of colorectal surgery at a single institution was analyzed.
SETTINGS: The study was conducted in a tertiary-referral medical center.
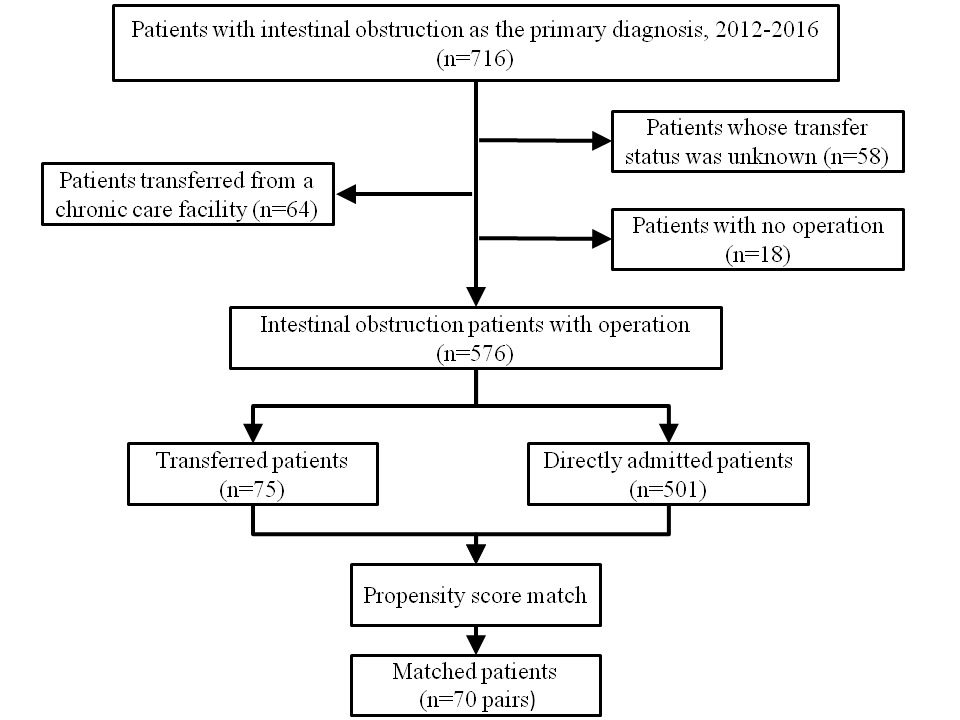
PATIENTS: Data for patients with the primary diagnosis of intestinal obstruction operated in the single institution's main campus from Jan 2012 to Dec 2016 were collected.
MAIN OUTCOME MEASURES: Preoperative characteristics and surgical outcomes (including intraoperative complication, postoperative complication, readmission, reoperation and postoperative 30-day mortality) were compared between transferred and directly admitted group, before and after propensity score match. Multivariate logistic regression was used to evaluate the impact of inter-hospital transfer on surgical outcomes.
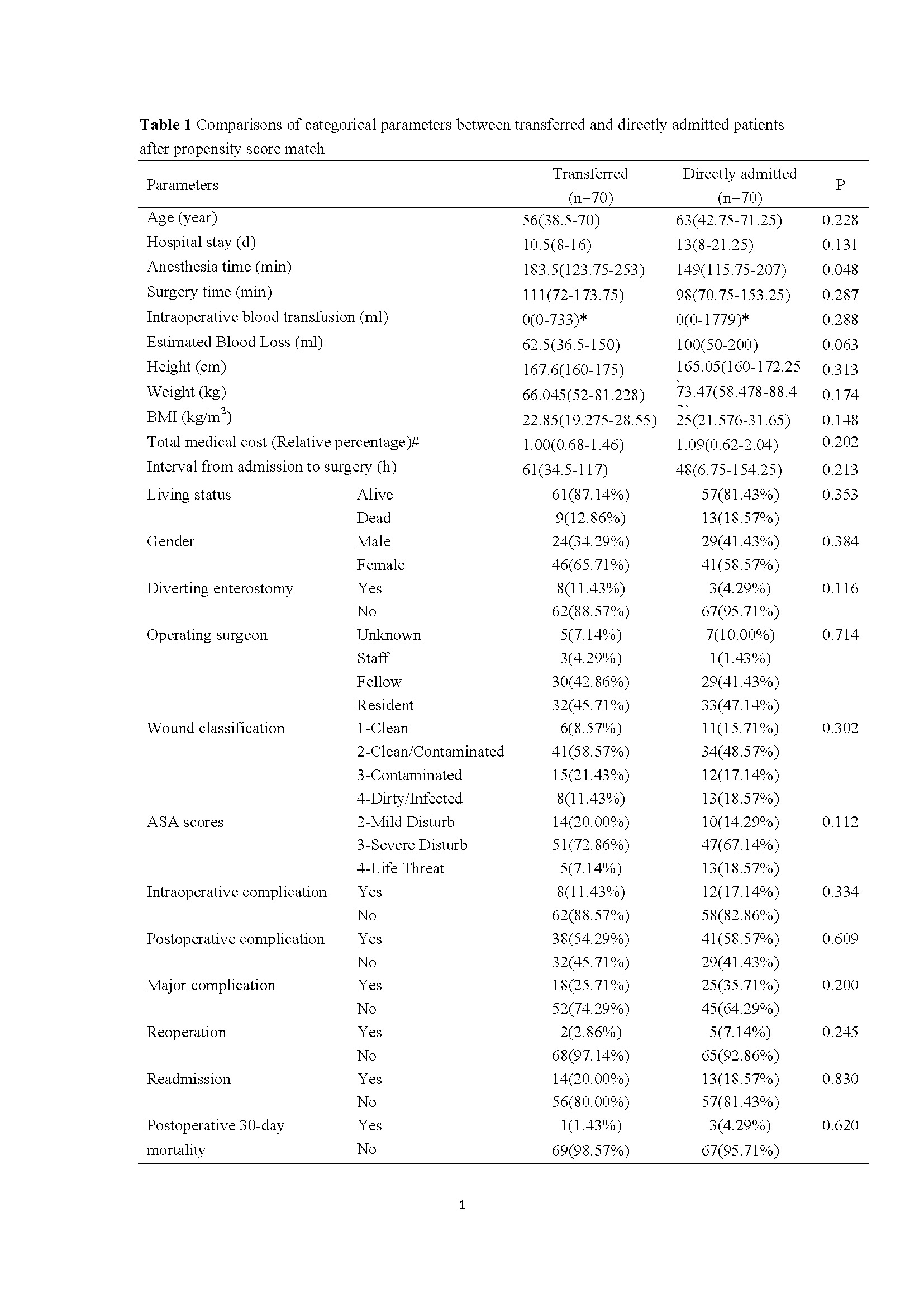
RESULTS: A total of 576 patients were included, with 75 in the transferred group and 501 in the directly admitted group. Before match, the transferred patients had longer waiting interval from admission to surgery (p < 0.001), more contaminated or infected wounds (P=0.021), different surgical procedures (P=0.021) and similar total medical cost (P=0.071), compared with the directly admitted group. Multiple logistic analyses showed that inter-hospital transfer was not independent predictor of any surgical outcome. After matching to balance the preoperative clinicopathological characteristics between the two groups, no differences were identified in all surgical outcomes and cost between the two groups (All P>0.05).
LIMITATIONS: We did not have the data of treatment and cost before transfer, and the reason of transfer.
CONCLUSIONS: Transferred emergent colorectal patients who undergo surgery have similar surgical outcomes and cost when compared to directly admitted patients undergoing similar procedures.
KEY WORDS: colorectal; intestinal obstruction; inter-hospital transfer; cost; complication; mortality.
Figure 1. Patient selection flow diagram
Figure 1. Patient selection flow diagram
Table 1 Comparisons of categorical parameters between transferred and directly admitted patients after propensity score match
Back to 2018 Posters
|