|
 |
Back to 2018 Posters
ISOLATING COELOMIC CAVITIES TO MANAGE CHOLEDOCHO-JEJUNO-TRANSPHRENIC-BRONCHIAL FISTULA IN LIVING DONOT LIVER TRANSPLANT RECIPIENT
Satjeet K. Deol*6, Harangad S. Bhangoo1, Prabh G. Singh7, Alyssa J. Meyer1, Zaheer H. Rizvi1, Eric S. Edell2, Deeksha K. Jandhala3, Fateh Bazerbachi1, Shanda H. Blackmon4, Janani S. Reisenauer5, Navtej S. Buttar1
1Gastroenterology, Mayo clinic, Rochester, MN; 2Pulmonary and Critical Care, Mayo Clinic, Rochester, MN; 3Infectious Disease Transplant, Mayo Clinic, Rochester, MN; 4Thoracic Surgery, Mayo Clinic, Rochester, MN; 5Interventional and Advanced Diagnostic Pulmonary Medicine, Mayo Clinic, Rochester, MN; 6Obstetrics and Gynecology, SPS Apollo Hospital, Sherpur Ludhiana, Punjab, India; 7Physiology, Government Medical College and Hospital, Chandigarh, India
Background and Aim: Living donor liver transplant recipients are at higher risk for bile leaks and bilomas. Acquired pathological communication between the biliary tract and the bronchial tree (broncho-biliary fistulae) or biliary tract and pleural space (pleuro-biliary fistulae) are rare and have not been reported in liver transplant patients. Subjecting these patients, with poor nutritional status, to complex surgery is high-risk. Our aim is to highlight a minimally invasive hybrid procedure used to successfully manage this complication
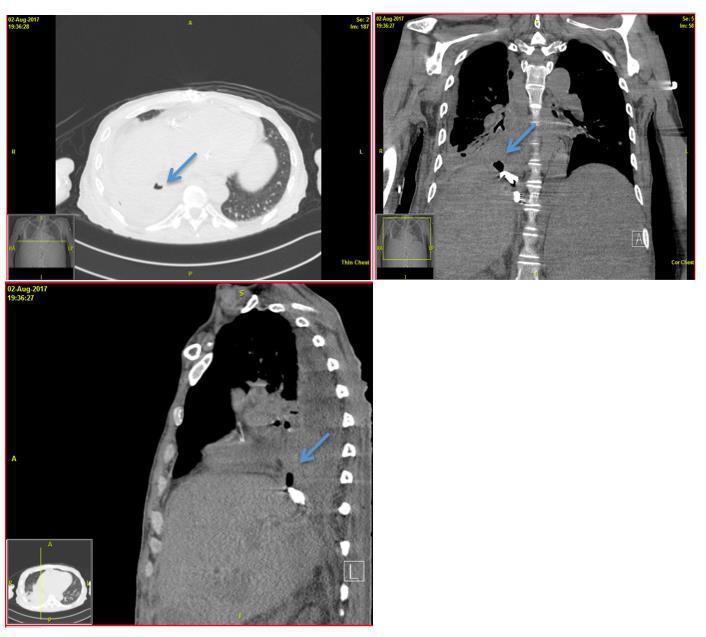
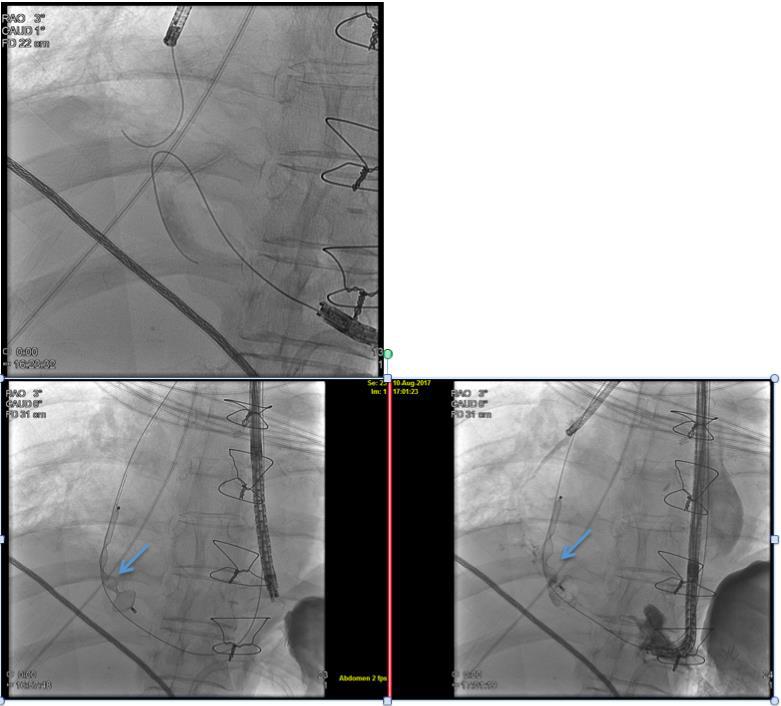
Method and Results: A 55 year old male with primary sclerosing cholangitis underwent living donor liver transplant and developed a chronic biloma after transplant. This was managed with percutaneous drainage and eventual indwelling trans-gastric double pig-tail stent placement. While on basiliximab and solu-medrol induction this patient developed worsening shortness of breath and cough containing bile. CT scan of the chest and abdomen revealed a loculated right pleural effusion, right lower lobe consolidation and a fistulous communication from choledocho-jejunal anastomosis, via the diaphragm, with the bronchial tree (Fig 1). Due to poor nutritional status and extensive infection, surgery was determined high risk. A hybrid interventional pulmonary and endoluminal approach was taken to pass a wire across the fistula and to abrade the tract. Using a Gooseneck microsnare (Amplatz GooseNeck® Microsnare by ev3 Endovascular, Inc. Plymouth, MN) a 15mm AVP-II vascular plug (Amplatz GooseNeck® Microsnare by ev3 Endovascular, Inc. Plymouth, MN) was carefully deployed across the diagram to isolate the thoraco-abdominal cavities (Fig 2). The patient reported immediate relief of their cough, was discharged home on antibiotics. Subsequent evaluation showed resolution of the pneumonia and pleural effusion and no evidence of the fistula. We have used a similar approach to manage nine additional patients with complex fistulas arising from various parts of the gastrointestinal tract and 7 out of 9 patients have demonstrated complete resolution of symptoms.
Conclusion: Hybrid minimally invasive interventions using biocompatible plugs are promising approaches to manage complex gastro-intestinal fistula and leaks and should be explored prior to complex high-risk surgery.
Figure 1: CT scan of chest and abdomen revealing the fistula and associated empyema depicted by arrow
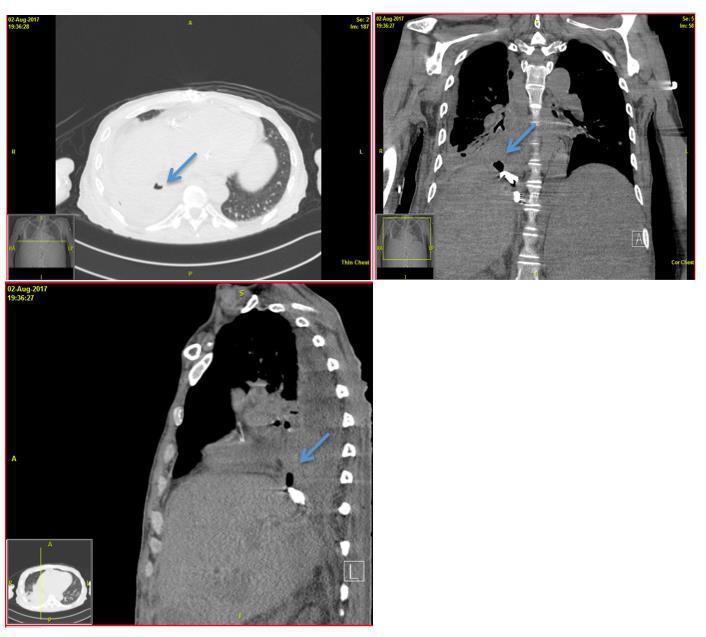
Figure 1: CT scan of chest and abdomen revealing the fistula and associated empyema depicted by arrow
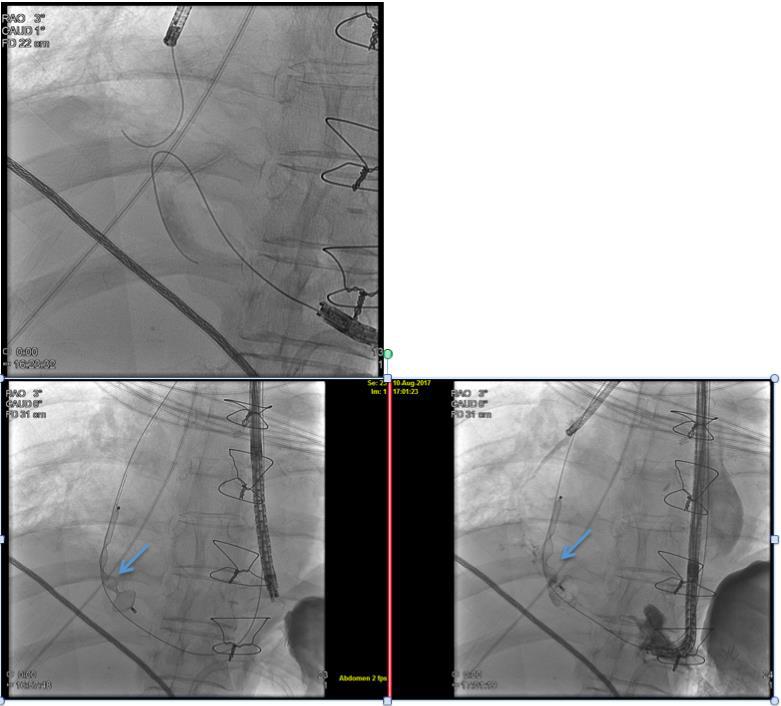
Figure 2: Isolation of thoracic and abdominal cavity with AVP-II plug using minimally invasive approach
Back to 2018 Posters
|