|
Back to 2018 Posters
IO US AND ICG GASTROSCOPY ARE MORE USEFUL THAN PREOPERATIVE COMMON HEPATIC ARTERY OCCLUSION FOR ASSESSMENT OF LIVER AND STOMACH BLOOD SUPPLY DURING DISTAL PANCREATECTOMY WITH CELIAC ARTERY RESECTION. EXPERIENCE OF 111 COMMON HEPATIC ARTERY CLAMPINGS AND 22 DP CARS
Viacheslav Egorov*2, Roman V. Petrov1, Julia A. Zhurina2
1Surgiacal oncology, Bakhrushin Moscow City Hospital, Moscow, Russian Federation; 2Radiology, Bakhrushin Brothers Moscow City Hospital,Russia, Moscow, Russian Federation
Aim. To study stomach and liver collateral arterial supply after common hepatic and celiac artery(CA) temporary occlusion.
Background. Distal pancreatectomy with celiac artery resection (DPCAR) is in use for borderline-resectable pancreatic cancer. It is believed that considerable reduction of the liver arterial supply after DPCAR may cause severe liver ischemia. Decision to reconstruct common hepatic or left gastric has to be justified.
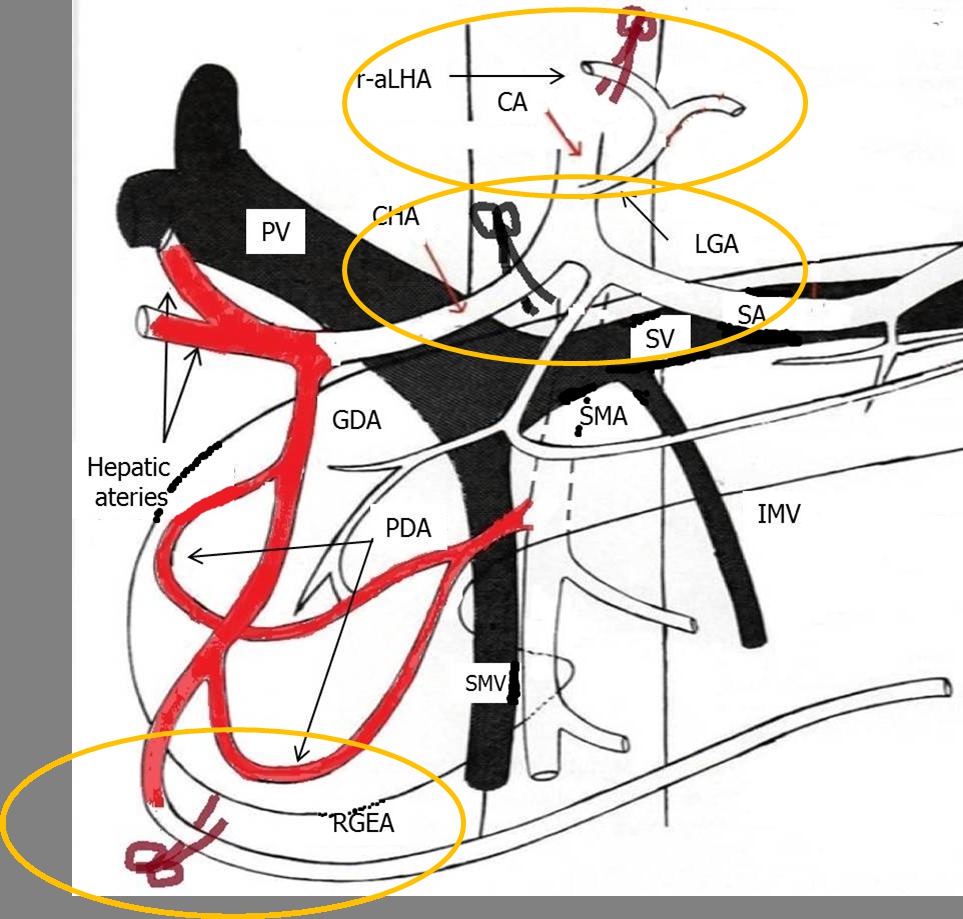
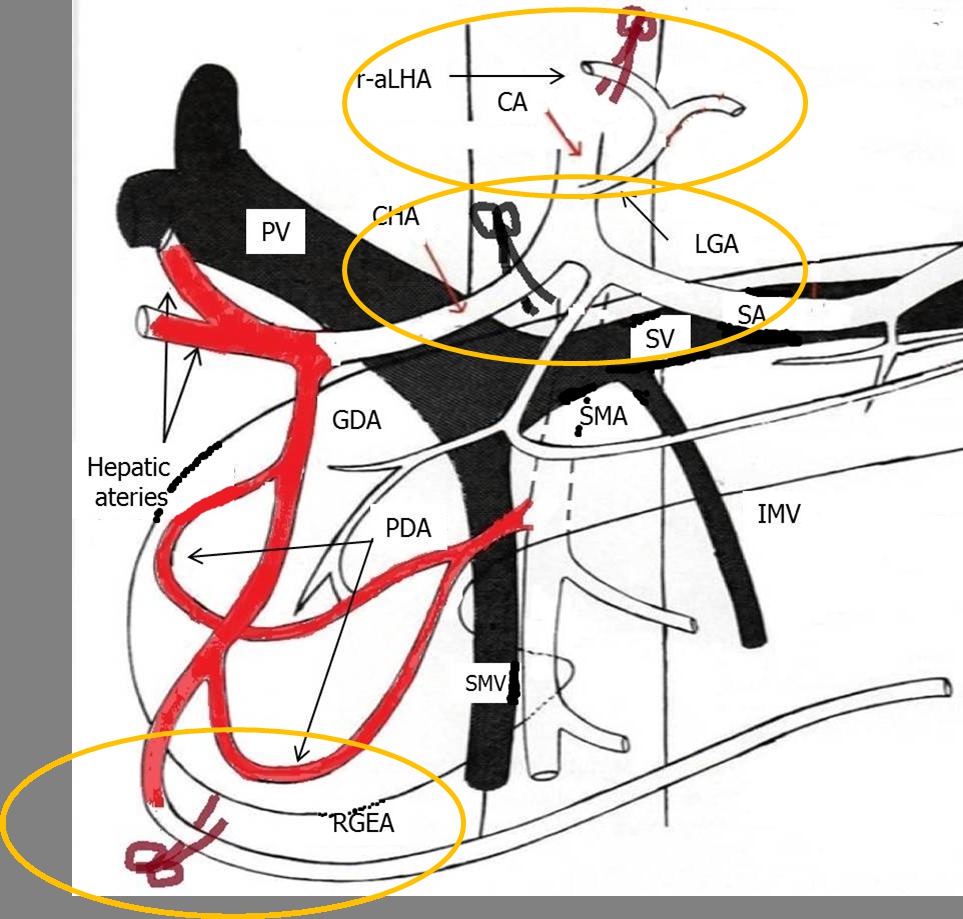
Patients and methods: Arterial anatomy, diameters of common, proper hepatic, gastroduodenal and pancreatoduodenal arcades(PDA) were registered before surgery in 111 consecutive patients with pancreatic body/tail cancer(n36), gastric cancer with pancreatic involvement(n30) and liver tumors(n45) by CT. For DPCAR(n22) patients ICG gastroscopy or CT were performed during or after surgery. Arterial blood flow in the liver and mean systolic velocity in hepatic arteries before and after clamping were measured intraoperatively by US (Fig.1).
Results: Classical arterial anatomy was identified in 67%. Pulse disappeared in 9(8%) cases after clamping of common hepatic, RGEA and aLHA/rLPA. Collateral arterial blood flow in the liver parenchyma was preserved in all cases. DPCAR led to increase of GDA, PDA and RGEA blood flow in 1-12 times; PDA were detected only once before DPCAR. Gastric ischemia was revealed in four and liver ischemia in 0 cases.
Conclusion:
1.IOUS is a reliable modality for intraoperative assessment of liver arterial blood supply during DPCAR;
2.Gastric ischemia is much more frequent event than liver ischemia after CA occlusion. IO ICG gastroscopy can be the option for the reconstruction of left gastric artery.
3. Common hepatic artery occlusion before DPCAR is unnecessary procedure.
Back to 2018 Posters
|