|
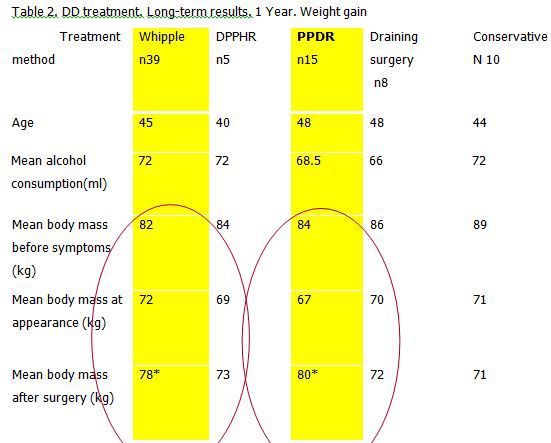
DOES IT MATTER WHICH NAME WE CHOOSE: DUODENAL DYSTROPHY, GROOVE OR PARADUODENAL PANCREATITIS? EXPERIENCE OF 77 CASES Viacheslav Egorov*, Roman V. Petrov Surgiacal oncology, Bakhrushin Moscow City Hospital, Moscow, Russian Federation Background: The term "paraduodenal pancreatitis"(PP) was proposed as an umbrella for cystic dystrophy in heterotopic pancreas (duodenal dystrophy,DD), paraduodenal cyst and groove pancreatitis, by reasoning that these conditions mimic pancreatic head tumors and share certain histological evidences. The reasons for amalgamation of these terms are unclear. Objective : To assess the results of different types of DD treatment. Method: 1.Prospective analysis of 77 cases of DD (2004-2017), comparing 77 pretreatment and 59 histopathological findings; 2.Assessment of clinical presentation and the results of DD treatment. Results: Preoperative diagnosis was correct in all the cases except one, when cystic tumor of the pancreatic head was suspected (1,8%). Patients were presented with abdominal pain(100%), weight loss(76%), vomiting(30%) and jaundice(18%). CT, MRI and endoUS were the most useful diagnostic modalities. Ten patients were treated conservatively, 35 underwent pancreaticoduodenectomies(PD), pancreatico- and cystoenterostomies(8), Nakao procedures(4), duodenum-preserving pancreatic head (DPPH) resections(5), and 15 pancreas-preserving duodenal resections(PPDR). No mortality. Full pain control was achieved after PPRDs in 93%, PDs in 83%, and after PPPH resections and draining procedures in 18% of cases. New diabetes mellitus(3) and exocrine insufficiency(3) developed after PD, Fig 1. Weight gain after 1 year was much more significant after PD and PPDR, Fig 2 . Conclusions: 1.The diagnosis of DD can be confidently determined preoperatively; 2.Early diagnosis of DD saves pancreas 3.Late diagnosis converts DD in PP and leaves patient only PD; 4.The efficacy of PPDR proves that DD is an entity of duodenal, but not paraduodenal origin. 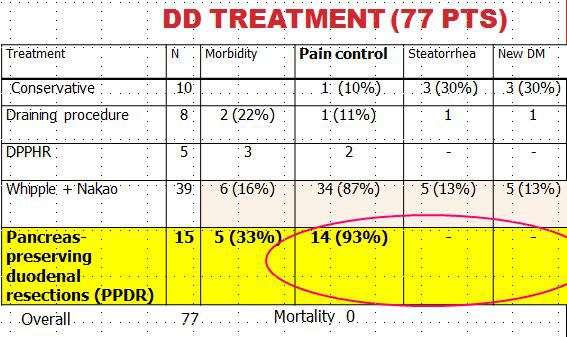
Back to 2018 Posters |
|||||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.