|
Back to 2018 Posters
PSEUDOACHALASIA IDENTIFIED DURING ATTEMPTED PERORAL ENDOSCOPIC MYOTOMY (POEM)
Kathryn A. Schlosser*1, Javier A. Otero1, John Hanson2, Brant T. Heniford1, Paul Colavita1
1Surgery, Carolinas Medical Center, Charlotte, NC; 2Gastroenterology, Carolinas Medical Center, Charlotte, NC
Background:
Accurate diagnosis of esophageal dysmotility is essential, as inappropriate intervention can devastate esophageal function. Here we describe a patient diagnosed with type II achalasia, found to have pseudoachalasia secondary to external compression of the gastroesophageal junction (GEJ) after orthotopic liver transplantation.
Patient Presentation:
A 60 year old female presented with one year of progressive dysphagia and postprandial regurgitation. Medical history was significant for chronic nausea since 2007, obesity with NASH, and liver failure since 2012. Liver transplant in 2013 was complicated by bile leak, sepsis and open abdomen. She had two remote esophageal dilations for unclear reasonss, eight gynecologic surgeries, and an open ventral hernia repair with mesh placement in 2014, in which the transplanted liver was noted to be "extraordinarily adherent to the edges of the costal margin and to the deep side of the diaphragm."
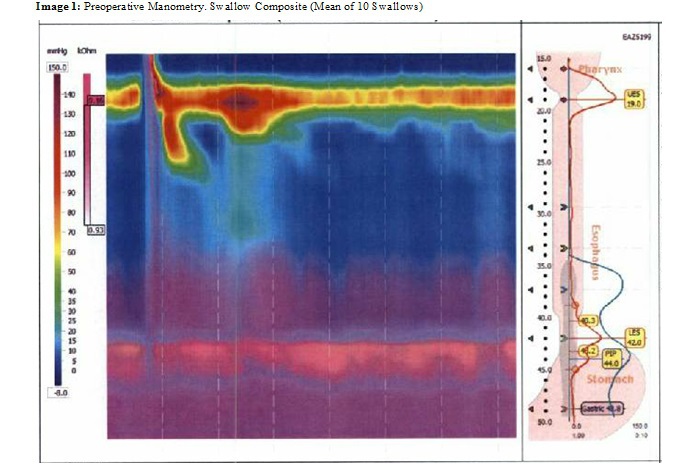
A dysphagia workup was performed. Endoscopy demonstrated mild esophageal dilation with food residue, and moderate chronic inflammation of the gastric antrum. Manometry revealed a lower esophageal sphincter (LES) mean pressure of 53.3mmHg with incomplete relaxation and integrated residual pressure of 25.1, 100% failed peristalsis with panesophageal pressurization (Image 1). Gastric emptying study showed mild delay during 1st and 2nd hours of imaging (6%, 25% respectively) with subsequent normalization. Upper GI showed esophageal dilation and contrast retention of the mid and lower thoracic esophagus. These findings were consistent with type II achalasia. Anticipating a hostile abdomen, peroral endoscopic myotomy (POEM) was selected to address her symptoms.
Intervention:
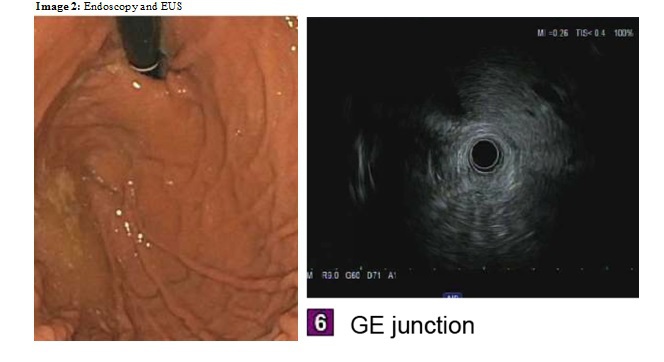
Initial endoscopy on the date of POEM revealed a dilated lower esophagus with retained food in the esophagus and gastric fundus. A 2-3 cm sliding hiatal hernia moved freely past a unilateral external obstruction. The obstruction was at the level of the LES or at the stomach, depending on the position of the sliding hiatal hernia. This was not consistent with achalasia, and POEM was abandoned. An empiric dilation was performed with a savary dilator with minimal resistance. The patient was then referred for endoscopic ultrasound (EUS) and possible stenting.
EUS demonstrated a patent lower esophageal sphincter with no sonographic abnormality of the GEJ, and located the liver as the source of extrinsic compression (Image 2). A stent was placed, but led to substantial discomfort and was removed after 2 weeks. The patient is being evaluated for thoracic crural release.
Conclusion:
Pseudoachalasia is most often associated with malignancy and can appear as achalasia during esophageal testing. Despite meticulous workup, the surgeon can be surprised by intraoperative findings. Recognition of pseudoachalasia can prevent inappropriate intervention.
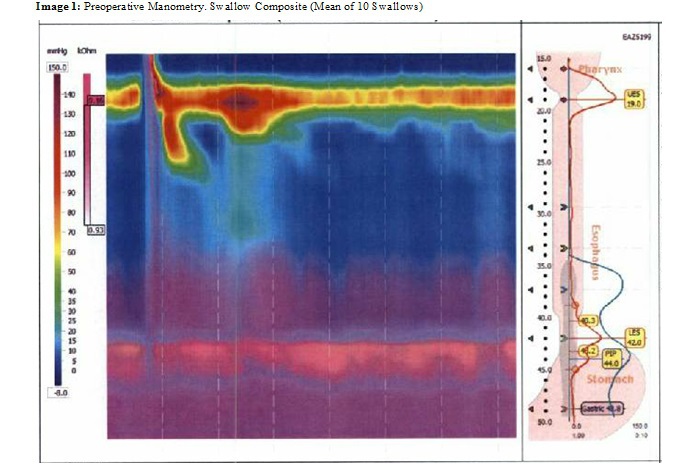
Image 1: Preoperative Manometry Swallow Composite (Mean of 10 Swallows)
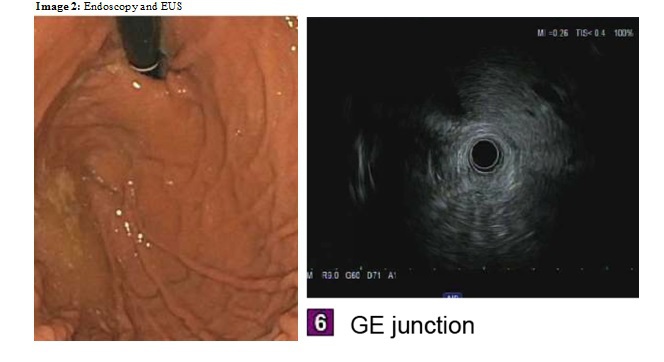
Image 2: Endoscopy and Endoscopic Ultrasound
Back to 2018 Posters
|