|
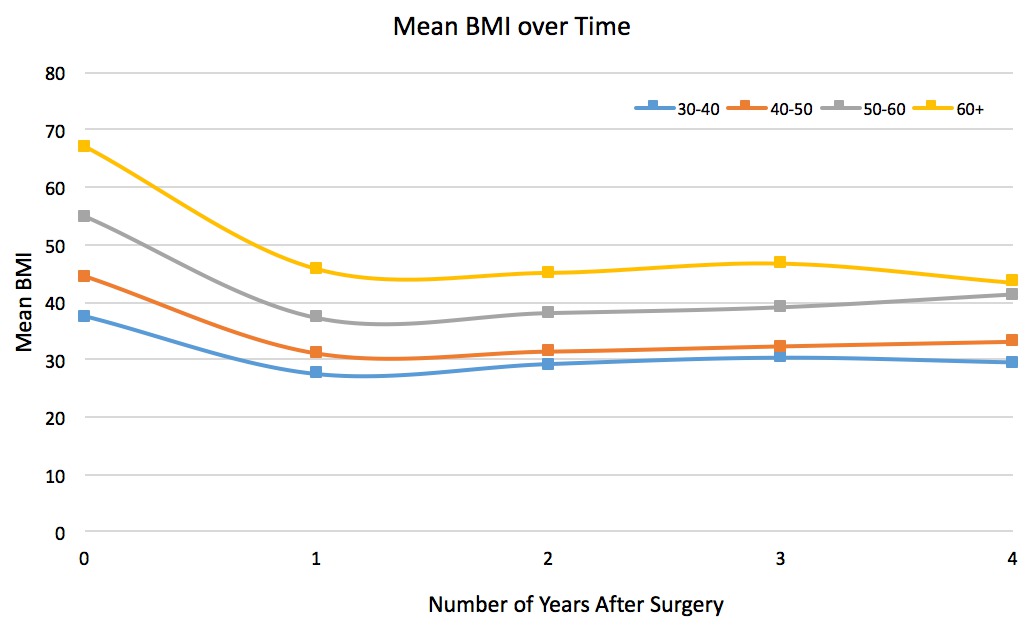
PRE-OPERATIVE BODY MASS INDEX PREDICTS WEIGHT LOSS TWO YEARS AFTER SLEEVE GASTRECTOMY BUT DOES NOT AFFECT COMORBIDITY RESOLUTION Katherine D. Gray*, Michael Y. Choi, Patrick T. Dolan, Gregory Dakin, Alfons Pomp, Cheguevera Afaneh Surgery, New York Presbyterian Hospital - Weill Cornell, New York, NY Background Laparoscopic sleeve gastrectomy (LSG) is the most commonly performed bariatric operation in the United States and has proven benefits up to five years in weight loss and resolution of obesity-associated comorbidities. Our aim was to stratify patients undergoing LSG at our institution based on pre-operative body mass index (BMI) and evaluate intermediate outcomes. Methods A prospective database is maintained of all patients undergoing bariatric surgery at our institution, a MBSAQIP Center of Excellence. Retrospective review was conducted of all patients undergoing primary LSG between 2004-2013. Patients were stratified based on their last recorded BMI prior to operation. Comorbidity resolution was measured by glycosylated hemoglobin (HgbA1c) for diabetes mellitus (DM) and number of oral medications for hypertension (HTN) and hyperlipidemia (HL). Percent excess BMI loss (%EBMIL) was used to evaluate weight loss. Results A total of 407 patients were stratified based on pre-operative BMI into BMI 30 - 39.9 (n = 56), BMI 40 - 49.9 (n = 171), BMI 50 - 59.9 (n = 116) and BMI ≥ 60 (n = 64); overall median BMI 48.1 (range 31.0 - 95.1). Age and American Society of Anesthesiology (ASA) score were linearly related to BMI strata, and patients in the highest stratum were younger (BMI ≥ 60: mean age 41.0 +/- 12.0 years versus BMI 30 - 39.9: mean age 47.3 +/- 13.5 years, p = 0.04) and more likely to be ASA Class 3 or 4 (90.7% of BMI ≥ 60 versus 58.9% BMI 30 - 39.9; p < 0.001). On logistic regression controlling for age, ASA classification, and diabetes, pre-operative BMI was the only independent predictor of thirty-day post-operative complications (OR 1.05, 95% CI 1.02 - 1.08, p = 0.003), readmission within ninety days of operation (OR 1.08, 95% CI 1.04 - 1.13, p < 0.001), and also approached significance as an independent predictor of leak (OR 1.07, 95% CI 0.99 - 1.14, p = 0.06). Mean follow-up was 26 months (range 1 - 112 months) with 65.3% of patients reaching one-year follow-up or greater. Comorbidity resolution was independent of pre-operative BMI (Table 1). Percent EBMIL varied by preoperative BMI at all time points; patients with a starting BMI 40-49.9 had the greatest %EBMIL at two years (66.3% +/- 17.2%) and patients with a starting BMI ≥ 60 had the least (52.7% +/- 14.7%), p < 0.001 between all groups. Similarly, initial BMI stratification was predictive of BMI at last followup (p < 0.001 between groups) (Figure 1). Conclusion Preoperative BMI is predictive of perioperative outcomes in LSG and can be used to predict BMI at intermediate follow-up. Sleeve gastrectomy is effective for control of metabolic comorbidities regardless of initial BMI. 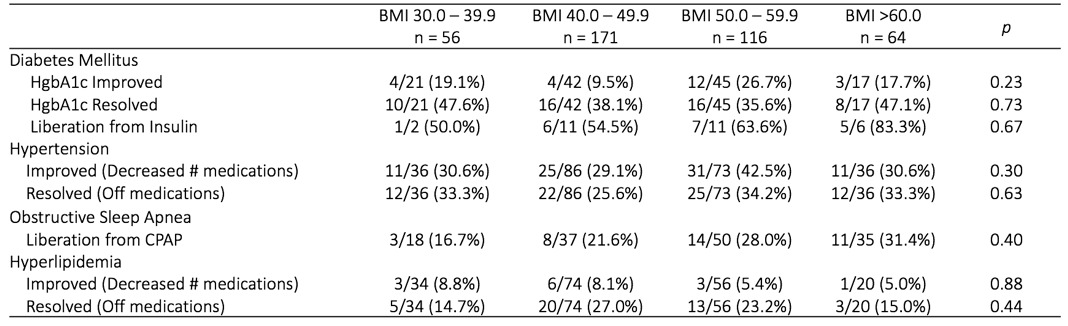
Table 1. Comorbidity resolution by pre-operative BMI. Back to 2018 Posters |
|||||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.