|
Back to 2018 Posters
INCREASING MORTALITY RATES WITH BARIATRIC REVISIONAL PROCEDURES: RESULTS OF A 10-YEAR NATIONWIDE SURVEY
Violeta Popov*2, Daniel Castaneda2, Marc Georgi3, Christopher C. Thompson1
1Brigham & Women's Hospital, Boston, MA; 2NYU School of Medicine, New York, NY; 3Catalyst Medical Consulting, Baltimore, MD
Bariatric surgery is the most effective and durable weight loss method. Data shows that mortality of primary procedures has decreased over the past 15 years. Bariatric revisional procedures have more than doubled during the same time period, and represented 13% of all bariatric surgeries in 2015. It is unclear if mortality rate has improved with this increased procedural volume.
Aims: To determine the trends in mortality and cost following inpatient bariatric revisional procedures over the past decade, and compare them to inpatient laparoscopic Roux-en-Y gastric bypass (RYGB) procedures.
Methods: This is a retrospective cohort analysis of the 2003, 2006, 2008, 2011 & 2014 Nationwide Inpatient Sample (NIS) discharge data on adult patients who had a principal diagnosis indicating a revisional bariatric surgery. The primary outcome was mortality following bariatric revisions. Secondary outcomes were total hospitalization charges, length of stay (LOS) and intensive care (ICU) stay, and mortality in the study group compared to inpatient RYGB. Univariate and multivariate logistic regression analyses were performed to identify independent predictors of mortality and common postoperative complications. Odds ratios, means and 95% confidence intervals are reported (95% CI).
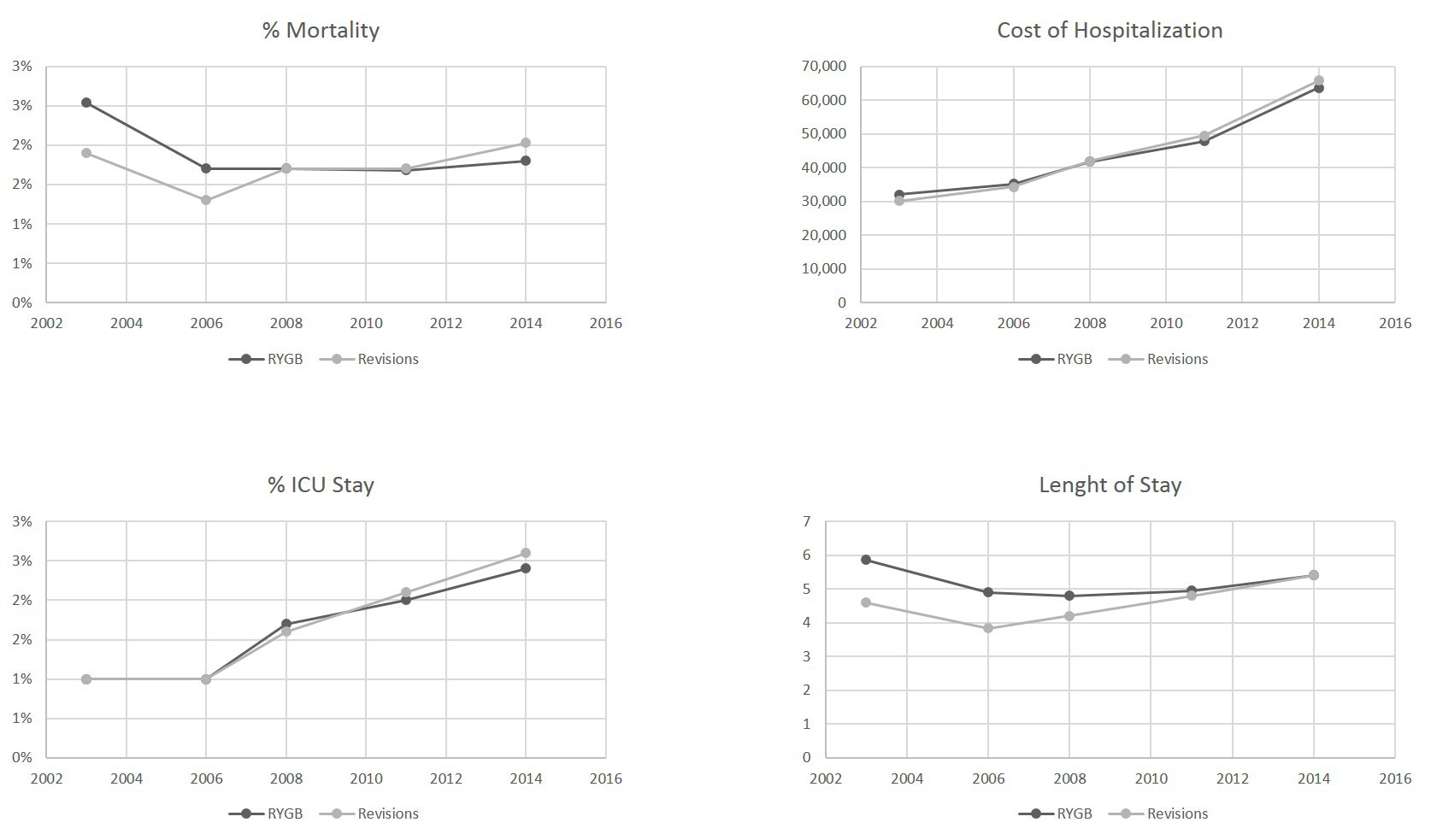
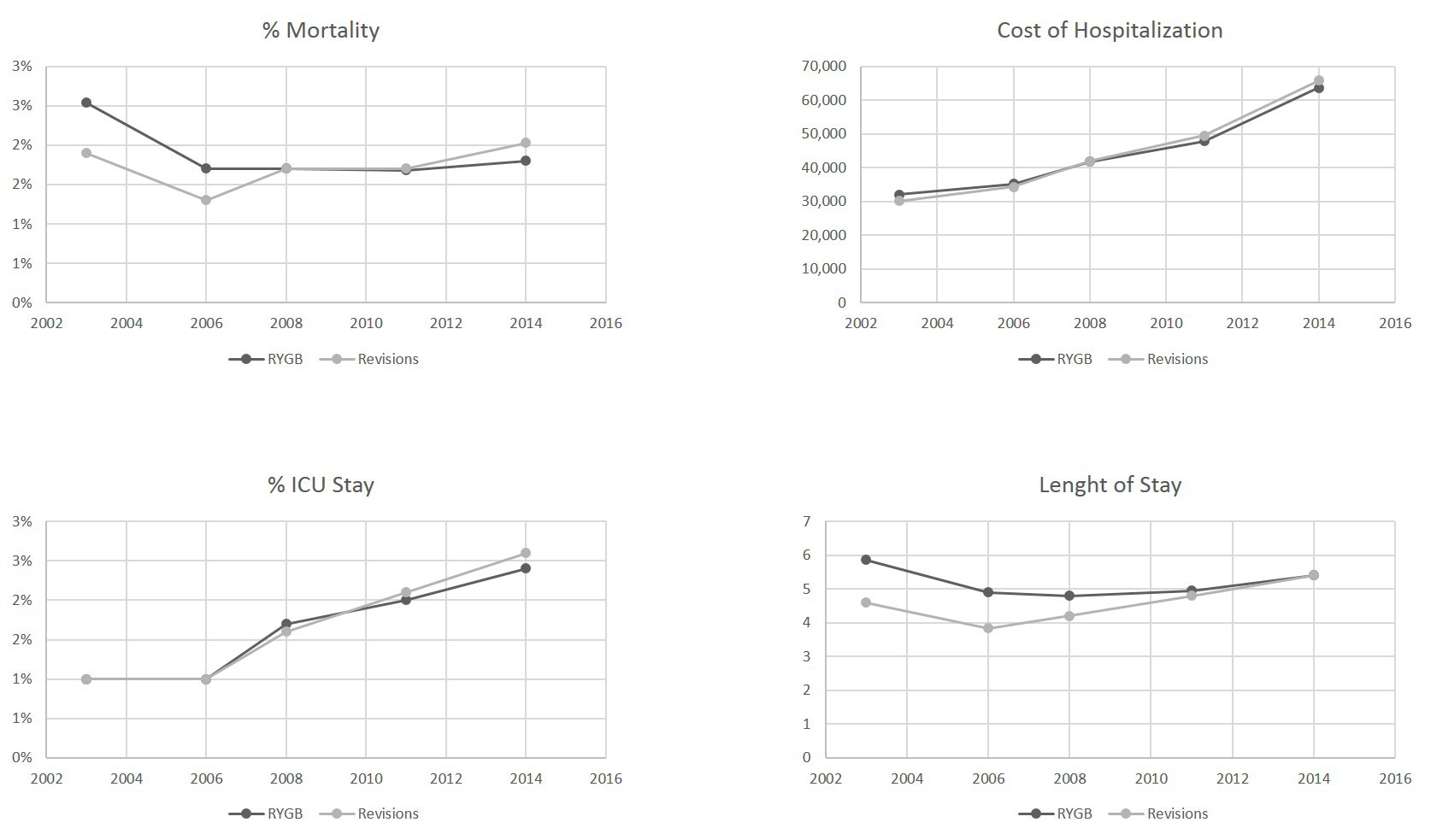
Results: A total of 130,538 patients who underwent inpatient bariatric revisional surgeries and 80,080 RYGB patients were included in the analysis. For RYGB, in-hospital mortality decreased from 2.54% in 2003 to 1.8% in 2014, and for revision, in-patient mortality increased from 1.9% to 2.03% in 2014, as shown in Figure 1. LOS increased from 4.6 days in 2003 to 5.4 days in 2014 for bariatric revisions, and decreased from 5.9 to 5.4 days for RYGB. Total cost for both procedures increased, from 30,000 in 2003 to 64-66,000 in 2014 (p<0.001 after adjusting for inflation). Percent of patient requiring intensive care increased for both procedures from 1% in 2003 to 3% in 2014 (Figure 1). Age, hospital size, teaching status, medical comorbidities (heart failure, kidney disease, hypertension, diabetes, coagulopathy) were significant predictors of revisional operations' mortality with multivariate regression.
Conclusion: Despite increasing bariatric revisional procedure volume, mortality has increased over time. During the same time period, inpatient mortality from initial RYGB has decreased, without differences in LOS or ICU admissions. These results may be due to a broad adoption of these procedures by less experienced surgeons. Further studies to investigate this ominous trend are warranted.
Back to 2018 Posters
|