|
Back to 2018 Posters
ENDOSPONGE-ASSISTED EARLY SURGICAL CLOSURE OF ILEAL POUCH-ANAL ANASTOMOTIC LEAKAGE IMPROVES LONG-TERM OUTCOMES
Karin Wasmann*1, Maud A. Reijntjes1, Merle Stellingwerf1, Cyriel I. Ponsioen2, Christianne J. Buskens1, Willem Bemelman1, Pieter Tanis1
1Department of Surgery, Academic Medical Center (AMC), Amsterdam, Netherlands; 2Department of Gastroenterology, Academic Medical Center, Amsterdam, Netherlands
Introduction:
For leakage of ileal pouch-anal anastomosis (IPAA), early surgical closure after endosponge treatment is highly effective in closing the anastomotic defect compared to conventional management (defunctioning ileostomy and drainage of the pelvic cavity). This study aimed to determine the long-term pouch function of ulcerative colitis (UC) patients after endosponge-assisted early surgical closure compared to those treated conventionally.
Method:
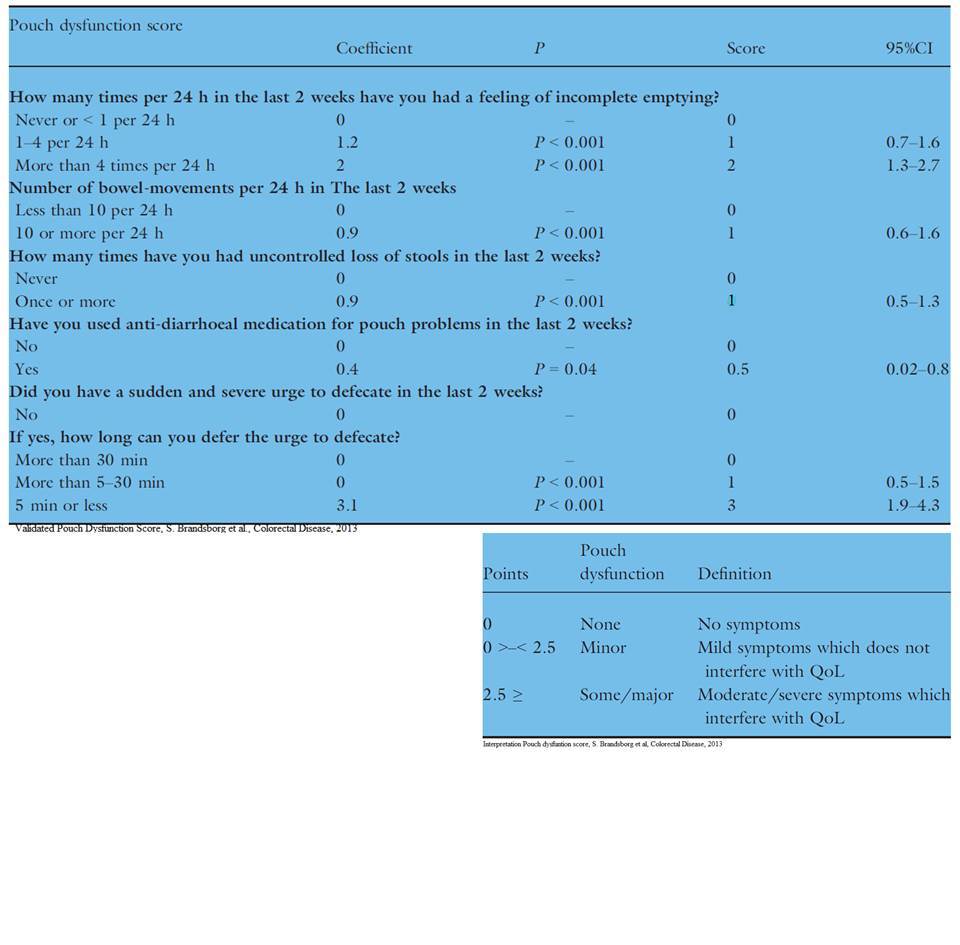
To all consecutive patients who underwent primary IPAA for UC between January 2002 and October 2016 a validated pouch dysfunction questionnaire was sent. From 2010 endosponge-assisted early surgical closure became the standard treatment for anastomotic leakage. It was hypothesized that endosponge-assisted early surgical closure compared to conventional treatment would improve long-term outcomes as it prevents chronic pelvic sepsis. The primary outcome was pouch function (none/minor, some/major dysfunction or pouch failure (ileostomy or pouch excision)). Secondary outcomes were anastomotic healing at 6 months, time to closure of anastomotic defect, and time to reversal of ileostomy.
Results:
A total of 305 patients underwent IPAA for UC, of whom 257 (84%) patients returned the pouch dysfunction questionnaire. Seventeen patients with an anastomotic leakage were treated with endosponge-assisted early surgical closure and 22 were treated conventionally. The control group included 218 patients. None/minor pouch dysfunction occurred in 59% vs. 43% vs. 65%, some/major in 35% vs. 38% vs. 30%, and pouch failure in 6% vs. 19% vs. 5% for early surgical closure, conventional treatment, and control group resp. (P0.07). Pouch failure was significantly lower in the early surgical closure and control group (6% and 5%, respectively) compared to conventional treatment (19%) (P0.03). Taking length of follow-up into account with Kaplan Meier analysis at 7.5 years (max. FU of the endosponge group) pouch failure occurred in 9%, 14%, and 5%, early surgical closure, conventional treatment, and control group, resp. (P0.2). Secondary anastomotic healing at 6 months was achieved in all patients in the early surgical closure group compared to two-third in the conventional treatment group (P0.01). Closure of anastomotic defect was achieved sooner in the early surgical closure group compared to the conventional treatment group, 8 (7-15) days vs. 76 (50-332) days, (P<0.001). Time to reversal of ileostomy was comparable between the early surgical closure and the conventional treatment group, 4 (2-6) months vs. 4 (3-13) months, (P0.4).
Conclusion:
Endosponge-assisted early surgical closure of anastomotic leakage of IPAA for UC is associated with improved long-term outcomes compared to conventional management of leakage.
Table 1. Pouch function & pouch failure
| | | None/minor dysfunction | Some/major dysfunction | Pouch failure | | | Type of treatment | n (%) | n (%) | n (%) | | | Leakage, early surgical closure | 10/17 (59%) | 6/17 (35%) | 1/17 (6%) | | | Leakage, conventional treatment | 9/21 (43%) | 8/21 (38%) | 4/21 (19%) | | | Control IPAA | 141/216 (65%) | 65/216 (30%) | 10/216 (5%) |
Fisher-exact test: pouch function P 0.07 & pouch failure P 0.02 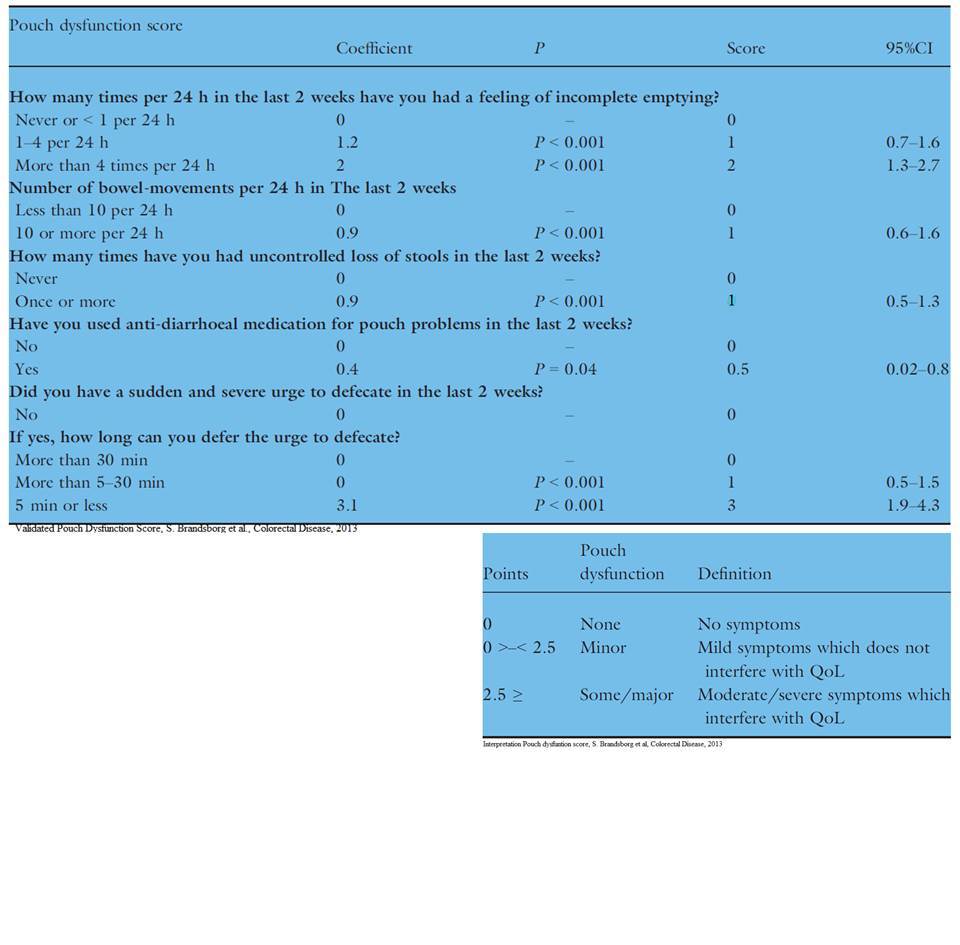
Back to 2018 Posters
|