|
Back to 2018 Posters
IS THERE A ROLE FOR DIVERTING LOOP ILEOSTOMY AFTER ILEOCOLIC RESECTION FOR CROHN'S DISEASE?
Nicholas P. McKenna*1, Amy E. Glasgow1, Elizabeth B. Habermann1, Eric Dozois2, Amy L. Lightner2
1Surgery, Mayo Clinic, Rochester, MN; 2Colon and Rectal Surgery, Mayo Clinic, Rochester, MN
Background: The use of a diverting loop ileostomy (DLI) to both prevent and reduce the severity of an anastomotic leak in low colorectal anastomoses is well established, but its efficacy following ileocolic resection for Crohn's disease (CD) remains unknown. The aim of this study was to investigate the impact of fecal diversion on the rate and severity of intra-abdominal sepsis in CD patients undergoing ileocolic resection and identify factors associated with surgeons' use of diversion following ileocolic resection.
Methods: A retrospective chart review of all patients undergoing ileocolic resection for CD at a single institution between July 2007 and August 2017 was conducted. Intra-abdominal sepsis was defined as either intraperitoneal abscesses or anastomotic leak and was graded using the Clavien-Dindo classification. For the evaluation of intra-abdominal sepsis, only type II (clean-contaminated) wounds were included for analysis of the role of DLI to prevent bias from contaminated or dirty fields. Patients not diverted and those with a DLI were included for analysis of factors associated with diversion. Univariate comparisons and multivariable logistic regression were conducted.
Results: 679 patients (369 female) with a median age of 37 years (range, 18-86) underwent ileocolic resection with primary anastomosis (537 type II wounds). The overall rate of intra-abdominal sepsis was 7% (N=39; 10% grade 2, 44% grade 3a, 26% grade 3b, 21% grade 4). In those with a DLI (n=26), 15% experienced intra-abdominal sepsis compared to 7% of those not diverted (n=511) (p=0.10). Reoperation for intra-abdominal sepsis was required in 75% of those with a DLI and in 43% of those not diverted (p=0.22). Of the 13 patients undergoing resection and end ileostomy, none developed intra-abdominal sepsis. Presentation with intra-abdominal sepsis was delayed in those with a DLI (median of 14 days [range 2-28]) compared to the group without diversion (median of 8 days [range 3-28]).
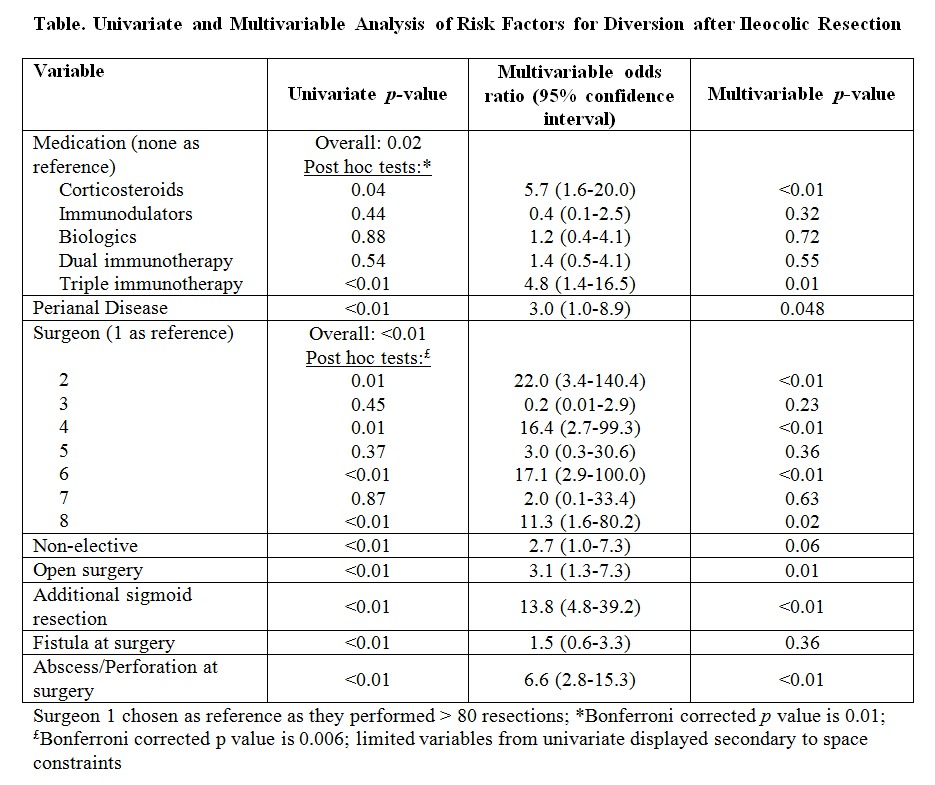
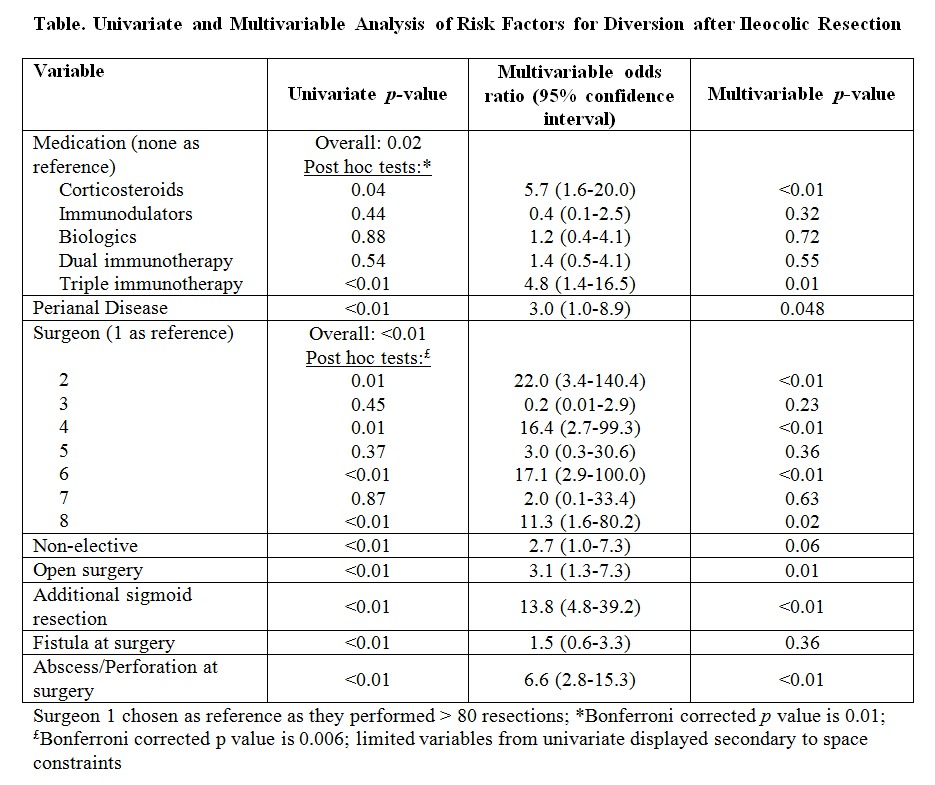
The decision to perform diversion was highly variable amongst individual surgeons with rates ranging from 0 to 16% for surgeons completing at least 37 resections. However, previously established risk factors for anastomotic leak were associated with the use of diversion on univariate analysis and multivariable analysis (Table).
Conclusion: These results suggest a diverting loop ileostomy did not reduce the rate of intra-abdominal sepsis or the need for reoperation following ileocolic resection. Resection and end ileostomy with restoration of intestinal continuity at a later date may better serve high-risk patients undergoing ileocolic resection. The use of diversion remains highly variable among individual surgeons.
Back to 2018 Posters
|