|
 |
Back to 2018 Posters
ANALYSIS OF PROGNOSTIC FACTORS AFTER RESECTION OF SOLITARY LIVER METASTASIS IN COLORECTAL CANCER - A 22-YEARS BICENTER STUDY
Sara Acciuffi1, Frank Meyer*1, Utz Settmacher2, Hans Lippert1, Roland Croner1, Annelore Altendorf-Hofmann2
1General Surgery, University Hospital Magdeburg, Magdeburg, Germany; 2General Surgery, University Hospital of Jena, Jena, Germany
Introduction In the last years, a large number of studies investigated predictors of outcome after hepatic resection for colorectal liver metastasis (CLM). The results reported are very heterogeneous and sometimes discording. We focused on a homogeneous group of patients characterized by solitary CLM treated with a curative (R0) resection.
Material and Methods : We recruited 350 patients with solitary liver metastasis of colorectal cancer at the University Hospitals of Jena and Magdeburg, who underwent curative liver resection between 1993 and 2014. All patients had follow-up until death or till summer 2016.
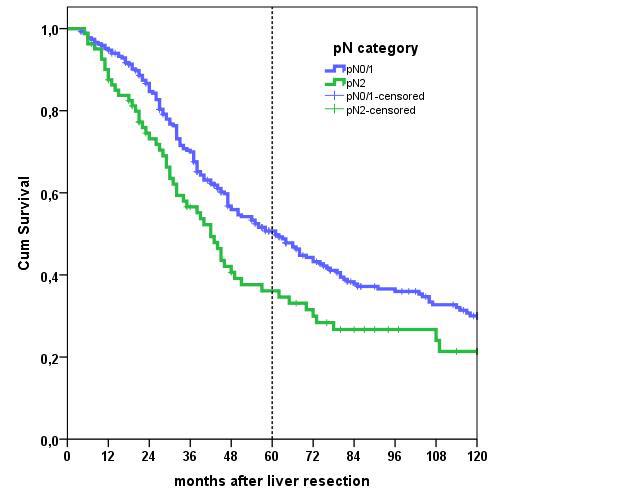
Results : The 5- and 10-year overall survival rates (OS) were 47% and 28%, respectively. The 5- and 10-year disease-free survival rates (DFS) were 30% and 20% respectively. These results are not that excellent as expected. The analysis of the prognostic factors revealed that pT category of primary tumour, size and grade of the metastasis and extension of the liver resection had no statistically significant impact on survival and recurrence rates.
The age of the patients, the involvement of more than three lymph node metastases by the primary tumour, synchronous metastasis, neoadjuvant chemotherapy and the presence of extrahepatic tumour showed a negative influence on the prognosis. Moreover, patient with rectal cancer had lower intrahepatic recurrence rate but a higher extrahepatic recurrence rate. In multivariate analysis age, status of lymph node metastasis at the primary tumour, location of primary tumour, time of appearing of the metastasis, the use of preoperative chemotherapy and the presence of extrahepatic tumour proved to be independent statistically significant predictors for the prognosis.
Conclusion : The long-term follow up of patients with R0-resected liver metastasis is multifactorial influenced. Age and comorbidity have a role only in the overall survival. More than three lymphnode metastasis at the primary tumour reduced both the overall- and disease-free survival. Extrahepatic tumour had a negative influence on the extrahepatic recurrence and on the overall survival. Neither overall survival nor recurrence rates were improved by using a neoadjuvant chemotherapy.
Table 1: Summary of Univariate analysis
| | p Overall survival | p Disease free survival | p Intrahepatic recurrence | p Extrahepatic recurrence | | Hospital | 0,117 | 0,949 | 0,668 | 0,257 | | Age | 0,007 | 0,575 | 0,301 | 0,790 | | Site of Primary tumour | 0,776 | 0,192 | 0,032 | 0,029 | | pT category | 0,316 | 0,090 | 0,087 | 0,599 | | pN category | 0,018 | 0,006 | 0,012 | 0,805 | | Grading | 0,241 | 0,372 | 0,990 | 0,485 | | Time of metastasis | 0,172 | 0,021 | 0,002 | 0,400 | | Neoadjuvant chemotherapy | 0,283 | 0,008 | <0,001 | 0,811 | | Size of metastasis | 0,119 | 0,243 | 0,789 | 0,352 | | Extrahepatic tumour | 0,018 | 0,004 | 0,417 | 0,009 | | Number of segments resected | 0,650 | 0,663 | 0,402 | 0,592 |
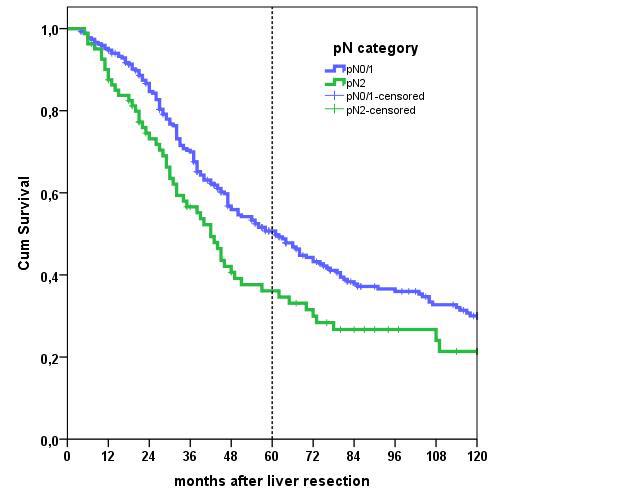 Figure 1: Observed survival rates dependent on pN category of primary tumour. Blue line: primary tumour with lymph node status pN0 or pN1. Green line: primary tumour with lymph node status pN2. Figure 1: Observed survival rates dependent on pN category of primary tumour. Blue line: primary tumour with lymph node status pN0 or pN1. Green line: primary tumour with lymph node status pN2.
Back to 2018 Posters
|