
|
PERITUMORAL CD3+ INFLAMMATION AND NEUTROPHIL TO LYMPHOCYTE RATIO PREDICT OVERALL SURVIVAL IN PATIENTS AFFECTED BY COLORECTAL LIVER METASTASES TREATED WITH SURGERY Matteo Maria Cimino*1, Matteo Donadon1, Domenico Mavilio2, Kelly Hudspeth2, Luca Di Tommaso3, Guido Torzilli1 1Department of General and Hepatobiliary Surgery, Humanitas Research Hospital & Humanitas University, Rozzano, MI, Italy; 2Department of Immunology, Humanitas Research Hospital & Humanitas University, Rozzano, Italy; 3Department of Pathology, Humanitas Research Hospital & Humanitas University, Rozzano, Italy
Background: systemic and local inflammation plays an important role in many cancers and colorectal liver metastases (CLM). While the role of local immune response mediated by CD3+ tumour infiltrating lymphocyte is well established new evidence on systemic inflammation and cancer such as neutrophil-lymphocyte ratio (NLR) are emerging. The aim of the study is to associate these two markers of inflammation to stratify patients affected by CLM in different overall survival (OS) and recurrence free survival (RFS) risk groups. 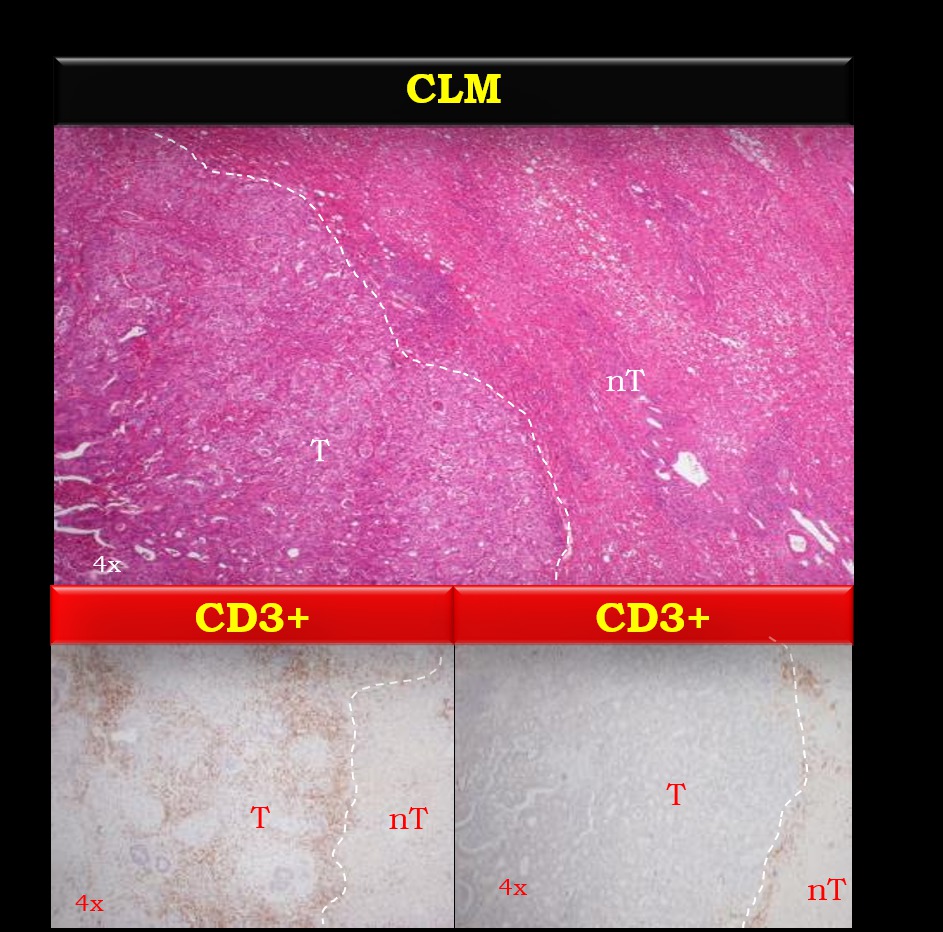
Back to 2018 Posters |
|||||||||||||||||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.