|
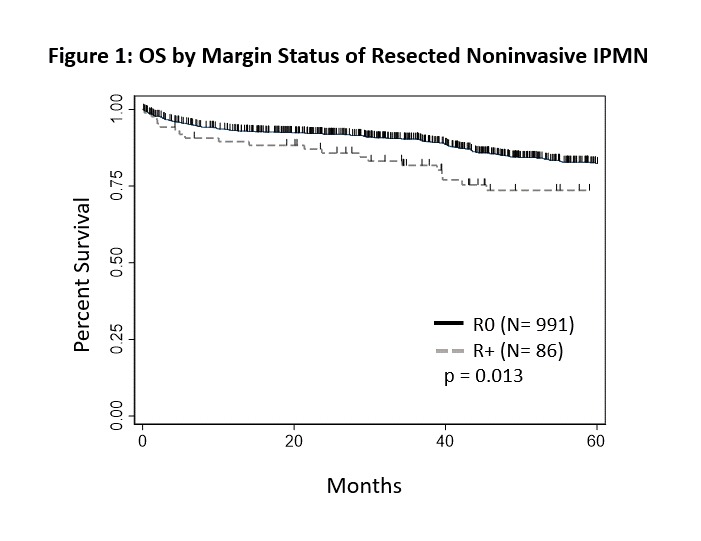
TOTAL PANCREATECTOMY FOR INTRADUCTAL PAPILLARY MUCINOUS NEOPLASMS DOES NOT WORSEN SURGICAL OUTCOMES: A NATIONAL CANCER DATABASE STUDY Benjamin Schmidt*, Ugwuji Maduekwe, C Tyler Ellis, Raphael Louie, Jen Jen Yeh, Karyn Stitzenberg, Michael O. Myers, Hong Jin Kim Surgical Oncology, University of North Carolina, Chapel Hill, NC Introduction: Total pancreatectomy for intraductal papillary mucinous neoplasms (IPMNs) is controversial. The 2012 international consensus guidelines for the management of pancreatic IPMNs suggest that the threshold for total pancreatectomy should be lowered for several indications including positive intraoperative margins, but acknowledges that this recommendation is based on weak evidence. To date, most studies are retrospective and limited to single centers. We selected patients with resected, non-invasive IPMN from the National Cancer Data Base (NCDB) to investigate choice of operation for IPMN without the additional influence of invasive disease on outcomes. Methods: Patients with resected noninvasive IPMN were identified in the NCDB (2004-2014). Student's t-test, Pearson's chi-square, Kaplan-Meier methodology and Cox regression were used where appropriate. Results: The NCDB included 1,099 patients with non-invasive IPMN and sufficient data for analysis. Patients with invasive IPMN (n=952), patients with insufficient surgical details (n=141) and patients with insufficient survival data (n=153) were excluded. This study included 163 patients (15%) who underwent total pancreatectomy, 273 patients (25%) who underwent distal pancreatectomy and 663 patients (60%) who underwent pancreaticoduodenectomy. There were no demographic or comorbid differences between groups, but patients undergoing total pancreatectomy had larger tumors (p= 0.005) and a trend towards longer pre-operative observation times (Table 1). Overall survival (OS) was similar for all operations (p=0.79 for total pancreatectomy v non-total pancreatectomy), with 5-year OS (95% CI) of 80% (77-88%) for total pancreatectomy, 84% (77-88%) for distal pancreatectomy and 81% (77-84%) for pancreaticoduodenectomy. There were no statistically significant differences between operations comparing 30-day readmission, 30-day mortality and 90-day mortality. Positive margin status on final pathology was associated with worse overall survival HR (95% CI) = 1.63 (1.10-2.41) across all operations (Figure 1). Conclusion: Choice of operation does not change short or long-term outcomes following resection of non-invasive IPMN, but positive margin status is associated with worse survival. Converting a limited resection to a total pancreatectomy in the setting of positive intraoperative margins for IPMN should be considered. This study has the limitations inherent to a large retrospective database study, and the morbidity of endocrine and exocrine insufficiency must also be measured into this decision. 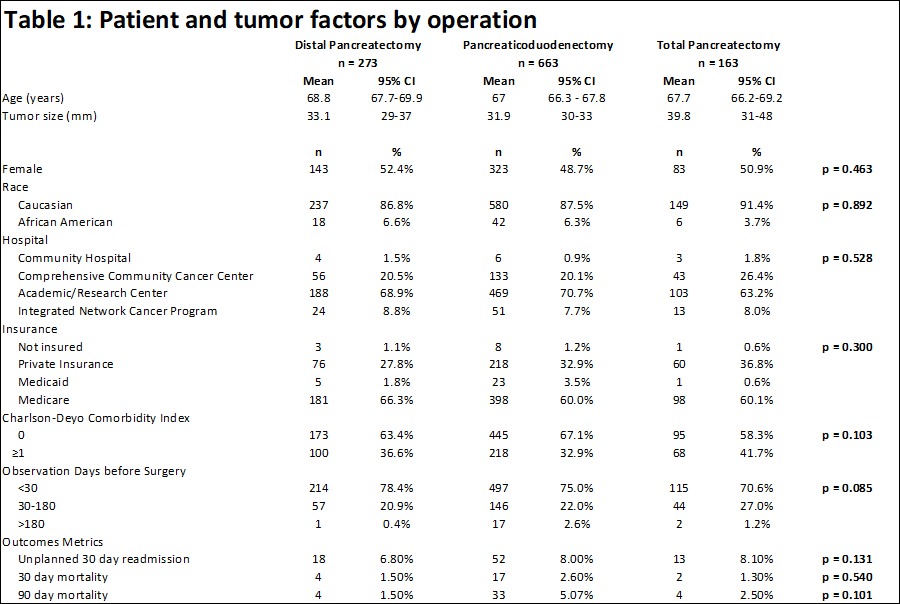
Back to 2018 Posters |
|||||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.