|
 |
Back to 2018 Posters
A NOVEL ENDOSCOPIC CLASSIFICATION SYSTEM TO ASSESS ESOPHAGOGASTRIC ANASTOMOTIC AND CONDUIT HEALTH FOLLOWING ESOPHAGECTOMY.
Sayak Ghatak*1, Karan Malhotra1, Michal J. Lada1, Edin Hadzijusufovic2, Thomas J. Watson3, Joseph Wizorek1, Christian Peyre1, Jeffrey Peters4, Carolyn Jones1
1Surgery, Thoracic Division, University of Rochester Medical Center, Rochester, NY; 2Surgery, University of Mainz, Mainz, Germany; 3Surgery, Medstar Health, Washington, ; 4Chief Operating Officer, University Hospitals, Cleveland, OH
Objectives: Anastomotic leak is one of the most common complications following esophagectomy, occurring in 5-40% of patients, and is associated with significant morbidity and mortality. The diagnosis of a leak most often relies on routine contrast esophagram, which has a poor sensitivity, or clinical suspicion. In this retrospective review, we evaluated the effectiveness of a novel classification system utilizing esophagogastroduodenoscopy (EGD) in the early assessment of anastomotic and gastric conduit health following esophagectomy and correlated with subsequent clinical outcomes.
Methods: The outcomes of patients who underwent routine EGD within two weeks of esophagectomy with esophagogastric anastomosis between January 1, 2003 and December 31, 2015 were reviewed. Anastomotic and gastric conduit health was classified as follows (Table): Grade I - healthy; Grade II -minor changes; Grade III - esophagogastric anastomotic ischemia/dehiscence; and Grade IV - gastric conduit ischemia/dehiscence. Outcomes including complications and stricture rates were collected and correlated to the grading of anastomotic health. Statistical significance was assessed using a 95% confidence interval, Pearson correlation coefficients (Ï?) and one-way ANOVA.
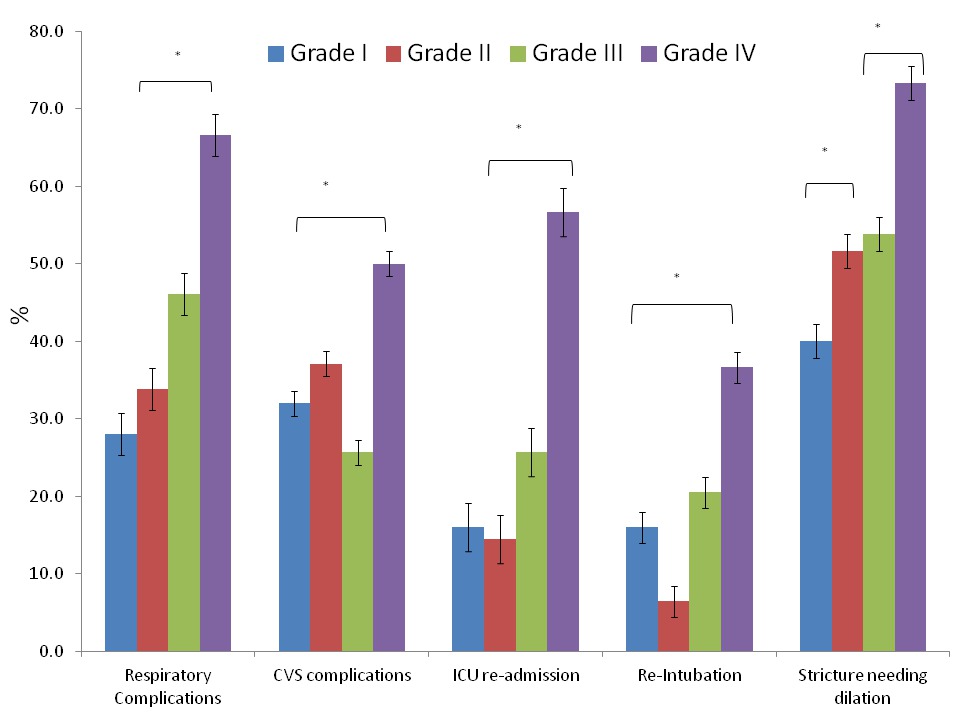
Results: Out of 421 patients who underwent esophagectomy, 156 (37%) patients underwent routine post-operative EGD at a median of seven days (range 3-14). Results of endoscopic assessment are shown in the Table. Complications directly related to the endoscopy occurred in 3/156 (2%) patients. Post-operative complications are shown in the Figure. There was a positive correlation with increasing rate of respiratory and cardiovascular complications (Ï? = +0.3) and stricture formation (Ï? = +0.2) with increasing severity of endoscopic grades (p value < 0.001).
Conclusions: Routine EGD following esophagectomy is a safe and effective tool for the evaluation of esophagogastric anastomosis and conduit health. We have defined a novel EGD based classification system that can aid in predicting post-operative complications and guide further clinical management.
Table: Endoscopic assessment of esophagogastric anastomosis and gastric conduit healing
| Grade | Classification | Endoscopic Findings | N (%) | | I | Unremarkable | No ischemia | 25 (16.0 %) | | II | Minor changes | Exudate, Debris, Eschar, Mucosal sloughing | 62 (39.7%) | | III | Major Anastomotic Changes | 39 (25.0%) | | A | Anastomotic Ischemia | 16 (10.3%) | | B | Anastomotic Dehiscence | 23 (14.7%) | | IV | Major Gastric Conduit Changes | 30 (19.2%) | | A | Conduit Ischemia | 22 (14.1%) | | B | Tip perforation, Staple line Dehiscence | 8 (5.1%) |
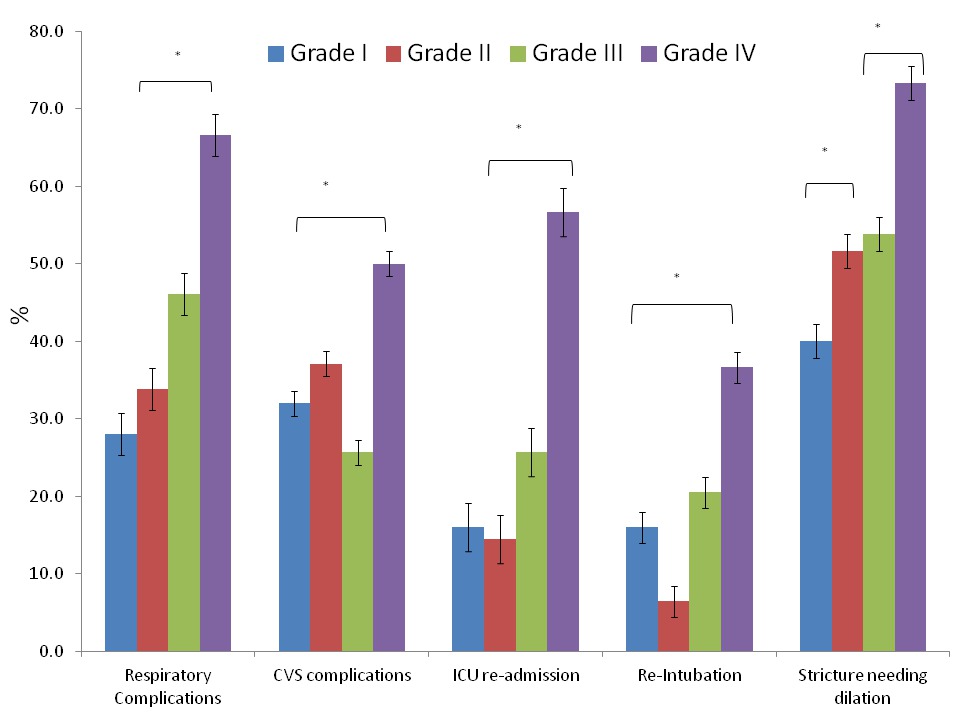 Post-operative complications in 156 patients who underwent routine EGD within 2 weeks of surgery.
Back to 2018 Posters
|