|
Back to 2018 Posters
COLONIC MYOELECTRICAL ACTIVITY MEASURED NON-INVASIVELY AFTER OPEN ABDOMINAL SURGERY PREDICTS TIME TO FIRST FLATUS/RESOLUTION OF POSTOPERATIVE ILEUS.
Anand R. Navalgund*1, Shyamali M. Singhal2, Khoi Tran2, Prithvi Legha2, Lindsay A. Axelrod1, Steve Axelrod1, George Triadafilopoulos3
1G-Tech Medical, Fogarty Institute for Innovation, Mountain View, CA; 2General Surgery, El Camino Hospital, Mountain View, CA; 3Gastroenterology and Hepatology, Stanford University School of Medicine, Palo Alto, CA
Background: Passage of flatus after abdominal surgery signals resolution of physiological postoperative ileus (POI) and often serves as the trigger to initiate oral feeding. Delayed passage of flatus is accompanied by abdominal pain, distention and nausea, in turn lengthening hospital stay and increasing resource utilization and costs. To date, there is no objective tool that can predict the time of POI resolution and potentially allow for early feeding.
Aims: We aimed to assess whether continuous noninvasive monitoring of gastrointestinal motor activity after abdominal surgery is feasible and can predict time to flatus.
Methods: Fifteen patients who underwent open abdominal surgery at a community hospital were enrolled between March 2016 and May 2017. Immediately following surgery, three novel wireless patches that acquire myoelectrical signals from the stomach, small intestine, and colon were placed on the anterior abdomen. The system transmits acquired data by Bluetooth to a custom app on an iPod Touch with a user interface to allow entering clinical events and other parameters. Post-processing of data included removal of large amplitude artifacts and band-pass filtering, followed by Fourier transformation to frequency space over selected time subintervals. Colon activity was calculated as the sum of the energy associated with the peaks in the 12 to 28 cpm range in the frequency space and then summed through the selected time subintervals.
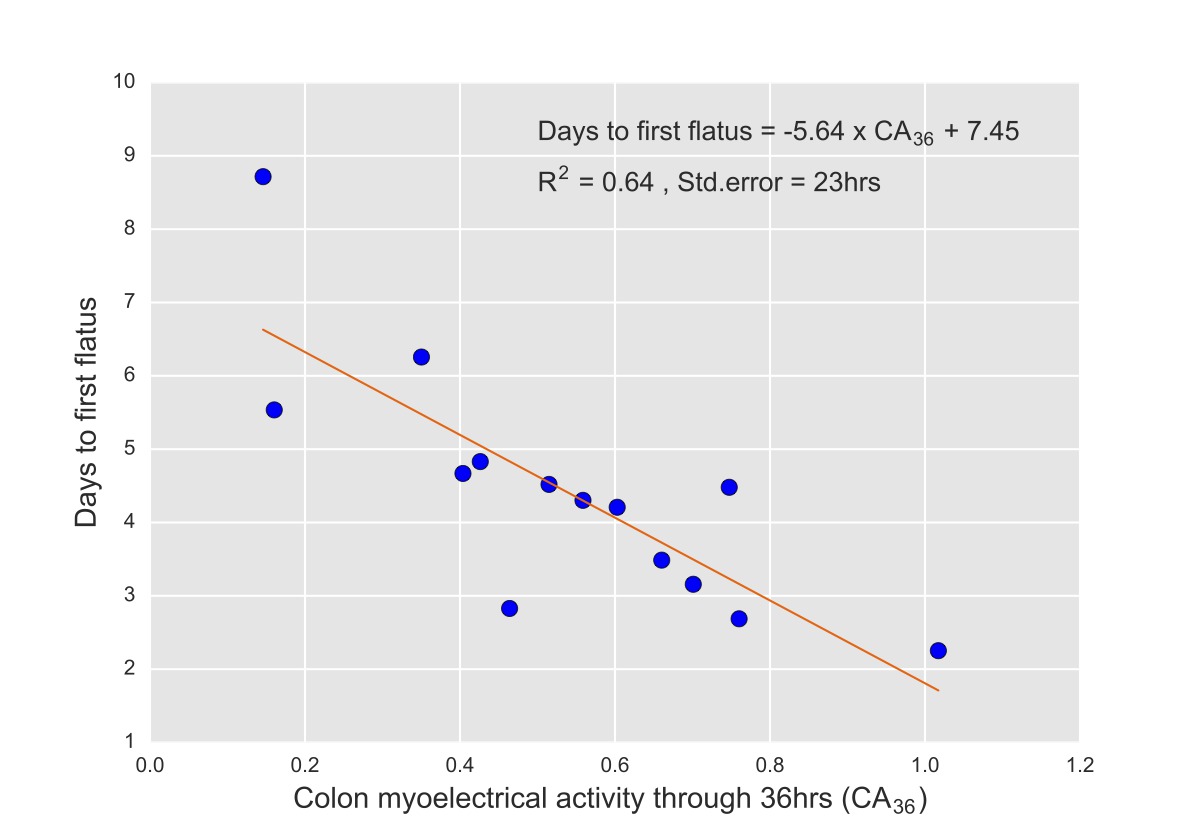
Results: Table 1 lists the characteristics of the 14 patients who were considered for the final analysis; one patient withdrew from the study. A simple linear regression was calculated to predict time to first flatus based on cumulative colonic myoelectrical activity at 36hrs (CA36) and a significant regression equation with an R2 of 0.64 was found (Figure 1). Participants predicted time to first flatus is equal to -5.64 x CA36 + 7.45, with a standard error of the estimate is 0.94 days (23 hrs). All patients were either on strict NPO or sips of water until they demonstrated passage of flatus. Hence, the first tolerated meal follows the first flatus and for 12/14 of them it was closely tied with their length of hospital stay (data not shown).
Conclusions: Non-invasive measurement of colonic myoelectrical activity after open abdominal surgery using a novel proprietary wireless patch system is feasible and predictive of the time of POI resolution up to 5 days (± 23hrs) in advance of its occurence. Such early prediction could optimize hospital care utilization by allowing for early feeding or delaying interventions. This tool can provide an objective measurement of specific interventions aimed at improving bowel function and quantify if an intervention is helpful. Upon further validation, we believe that this technology may soon guide patient management within the Enhanced Recovery After Surgery (ERAS) protocols.
Table 1. Patient characteristics
| ID | DEMOGRAPHICS | PROCEDURE | DAYS TO FIRST FLATUS | DAYS TO DISCHARGE | | 1 | 91 M | Ileocolectomy | 4.5 | 24 | | 2 | 70 F | Colostomy reversal | 8.7 | 11 | | 3 | 74 M | Whipple | 4.6 | 31 | | 4 | 82 F | Colostomy reversal | 4.8 | 6 | | 5 | 68 M | Liver and Colon resection | 6.2 | 9 | | 6 | 72 M | Lower anterior resection | 2.8 | 6 | | 7 | 33 M | Ileocolectomy | 3.1 | 8 | | 8 | 48 M | Colostomy reversal | 3.4 | 5 | | 9 | 52 F | Hemicolectomy | 4.2 | 9 | | 10 | 60 F | Ventral Hernia repair | 2.6 | 5 | | 11 | 83 F | Liver resection | 4.3 | 7 | | 12 | 69 M | Whipple | 4.4 | 11 | | 13 | 84 M | Sigmoid colectomy | 2.2 | 7 | | 14 | 33 M | Distal Pancreatectomy | 5.5 | 13 |
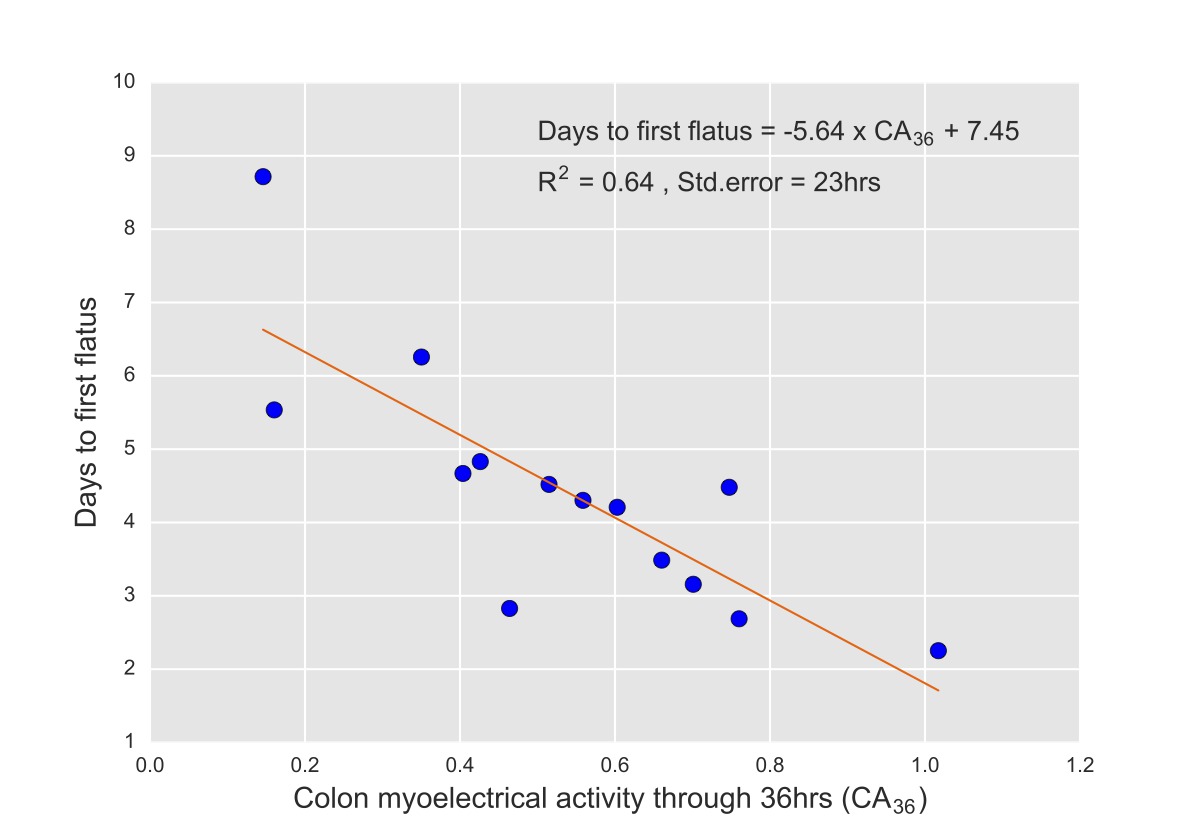 Figure 1.
Back to 2018 Posters
|