|
 |
Back to 2018 Posters
ENDOSCOPIC RESTORATIVE ANASTAMOSIS FOR FISTULA THERAPY (ENDO-RAFT), A NOVEL ALTERNATIVE FOR ILEOVAGINAL FISTULA IN THE SETTING OF CARCINOMATOSIS
Alyssa J. Meyer*1, Zaheer H. Rizvi1, Harangad S. Bhangoo1, Prabh G. Singh2, Satjeet K. Deol3, Barham K. Abu Dayyeh1, Navtej S. Buttar1
1Gastroenterology, Mayo clinic, Rochester, MN; 2Physiology, Government Medical College and Hospital, Chandigarh, India; 3Obstetrics and Gynecology, SPS Apollo Hospital, Sherpur Ludhiana, Punjab, India
Background: Fistulas & leaks are devastating complications that result in significant morbidity & mortality. In the setting of peritoneal carcinomatosis (PC), particularly from endometrial carcinoma extrinsic bowel obstruction occurs up to 10% patients. Proximally dilated bowel in the setting of pelvic surgery & staple line provides an undesirable decompressive portal via other pelvic viscera. Incomplete decompression & associated fecal contamination has mortality rates up to 16%. Our aim is to highlight response to conventional surgical & endoscopic intervention & explore the novel endoscopic techniques to provide minimally invasive alternate when convectional approaches are felt to be high-risk
Methods & Results: In 82 patients [54 females & 28 males; mean age 61] who received treatment for PC, 80% had poorly differentiated cancer & 60% had poor ECOG status (≤2). Equal number of patients underwent surgery or stenting (43.9 & 47.5 respectively). Patients were comparable in two groups as far as age, gender, type of malignancies, histological tumor grade & ECOG. Survival (in weeks) was found to be similar in patients who underwent primary stenting & primary surgery (25(10.3 - 39.6) vs. 19(5.7 - 32.3), p=0.183), however duration of hospitalization was shorter for patients primarily undergoing stenting (4.35±5.53 days vs. 8.02 ±6.67 days, p=0.011). Stent placement was clinically successful in 79.5% cases but durable clinical response was only noted in 59% patients. The case outlined in Figure1 was a 53-year-old female with Stage IV, high grade endometrioid adenocarcinoma with a sigmoid obstruction that was not amenable to stent placement & it was associated with large volume intestinal leakage via the vagina with second degree skin burn. The entire process was further complicated by a necrotic abscess cavity with severe lower abdominal pain, which was poorly controlled by patient controlled analgesia. Given the aforementioned data, patient & the team requested a consideration for alternate minimally invasive approach. To address this issue, the existing fistula & abscess cavity were exploited to create EUS assisted novel ileo-rectal anastomosis with a fully covered stent as outlined in the Figure1 below. Patient noticed remarkable recovery of her symptoms within a few days, her skin improved & she required only a minimal dose of pain medication for overall symptom control. The patient remained completely asymptomatic from GI leakage per the vagina or pain & was able to manage her stool frequency via the rectum till she succumbed to the extensive metastatic disease
Conclusion: Management of PC is challenging with limited durable symptomatic response either with surgery or luminal stenting. We show a novel, minimally invasive alternate technique with anastomosis creation between the intestine & rectum to greatly improve patient symptoms & quality of life
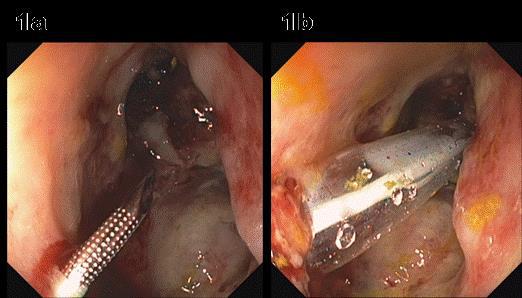
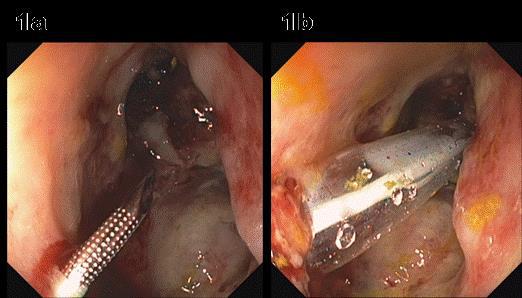
Figure 1: A) 19-guage needle from midrectum through abscess cavity under Alpha 10 echolinear ultrasound guidance, B) A stiff Jagwire was maneuvered from the rectum into the cavity & through the fistula into the intestine to dilate the tract for stent placement.
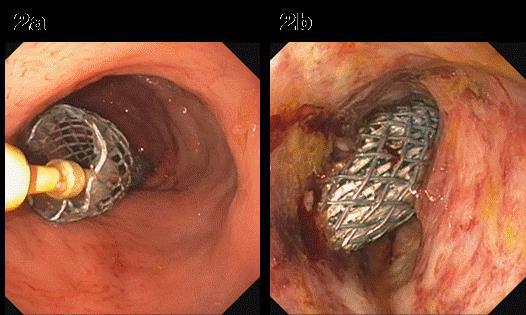
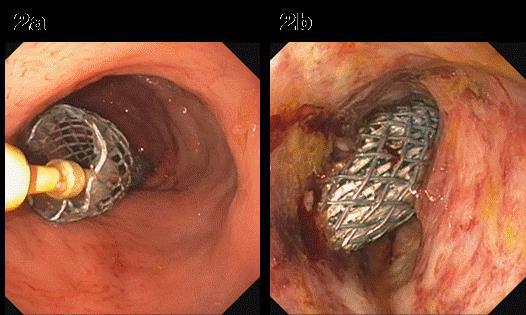
Figure 2: A & B) A partially covered WallFlex stent (18mm X 123mm) was deployed in a fashion that the covered portion bypassed the cavity. A novel communication was created between the small intestine & rectum via the abscess cavity to bypass the abscess cavity as well as cavity to vagina fistula.
Back to 2018 Posters
|