|
 |
Back to 2018 Posters
HOSPITAL VOLUME IS A SIGNIFICANT PREDICTOR OF LENGTH OF STAY FOLLOWING RECTAL CANCER SURGERY.
Katerina O. Wells*1, Gilder E. Richard2, Walter Peters1, James W. Fleshman1
1Surgery, Division Colorectal Surgery, Baylor University Medical Center, Dallas, TX; 2Dept. of Clinical Trials, Baylor Scott & White Research Institute, Dallas, TX
Introduction: Rectal cancer surgery is a complex surgical procedure and data suggests that outcomes are improved when performed in high volume centers. As such, there is a trend toward centralization of care in an effort to optimize outcomes. Nevertheless, rectal cancer surgery continues to be performed in low-volume centers with varying quality. The purpose of this study is to identify predictors of the quality indicator, length of stay (LOS), following rectal cancer surgery.
Methods: This is a retrospective review of the Dallas-Forth Worth Hospital Council's (DFWHC) QlikView system of all rectal cancer surgeries performed at participating hospitals. All admissions with ICD9 and ICD10 rectal cancer surgery diagnosis codes were queried over 2015Q1-2017Q1. The DFW Inpatient Analysis was used to determine the primary outcome of LOS, hospital volume, and patient-related factors including risk of mortality (ROM), severity of illness (SOI), and Elixhauser comorbidities. Spearman's Rho Correlation was determined for LOS and hospital volume. Binary Logistic Regression and CHAID modeling was performed using patient attributes as independent variable predictors of LOS beyond a threshold of 75th percentile (8 days).
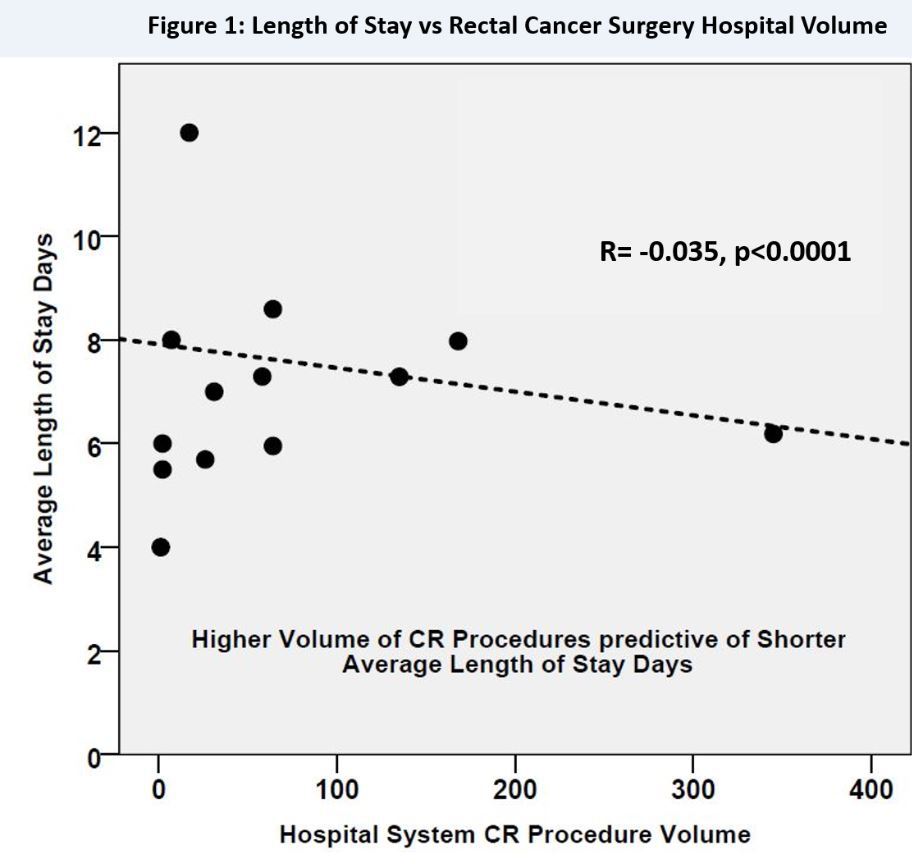
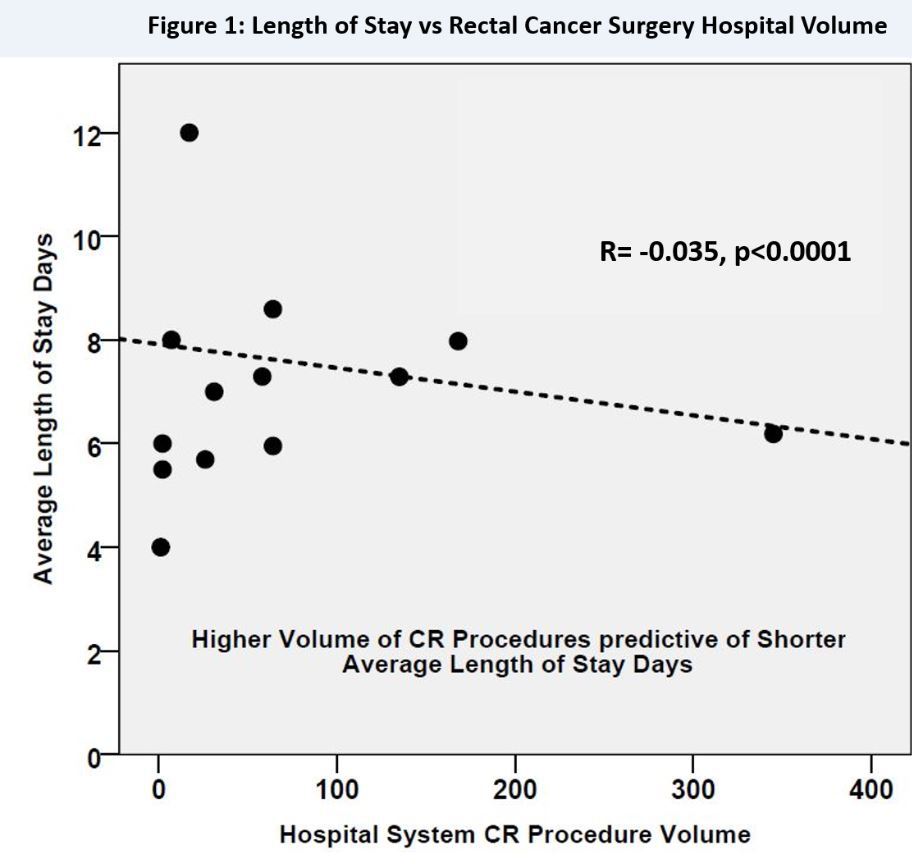
Results: Nine-hundred twenty encounters of rectal cancer surgery were identified over the time period. Median LOS was 5.3 days. There is a significant inverse correlation between LOS and hospital volume of rectal cancer surgery (R=-0.0350, p<0.0001). Additional independent predictors for prolonged LOS beyond a threshold of the 75th percentile LOS (8 days) include extreme ROM and SOI scoring (OR 47.3, 95%CI 6.0-366.6, p<0.0001), Emergency surgery (OR 5.5, 95%CI 2.7-11.2, p<0.0001), Age 70-74 yrs. (OR 1.8, 95%CI 1.1-3.1, p=0.024), and Elixhauser Comorbidity Diagnoses (ECD) of anemia (OR 1.8, 95%CI 1.1-3.0, p=0.017), electrolyte disturbance (OR 2.3, 95%CI 1.5-3.6, p<0.0001), and weight loss (OR 4.2 95%CI 2.1-8.2, p<0.0001).
Conclusion: High volume centers demonstrate significantly reduced LOS following rectal cancer surgery, which is a positive quality indicator. Patients at highest risk for prolonged length of stay are those presenting with emergency indications, acute cancer related comorbidities of weight loss, anemia and electrolyte disturbance, and those considered to have extreme or major ROM and SOI. It is likely that these patients are best managed in high volume centers in order to optimize quality outcomes.
Table 1: Binary Logistic Regression of 75% percentile (8 days) LOS
| Variables | OR (95%CI) | p value | | Extreme Risk of Mortality and Extreme Severity of illness | 47.3 (6.0-366.6) | <0.0001 | | Major Risk of Mortality and Major Severity of illness | 6.8 (3.6-12.5) | <0.0001 | | Emergency case | 5.5 (2.7-11.2) | <0.0001 | | Age 70-74 | 1.8 (1.1-3.1) | 0.024 | | Elixhauser comorbidity Anemia | 1.8 (1.1-3.0) | 0.017 | | Elixhauser comorbidity Electrolyte disturbance | 2.3 (1.5-3.6) | <0.0001 | | Elixhauser comorbidity Weight loss | 4.2 (2.1-8.2) | <0.0001 |
Back to 2018 Posters
|