|
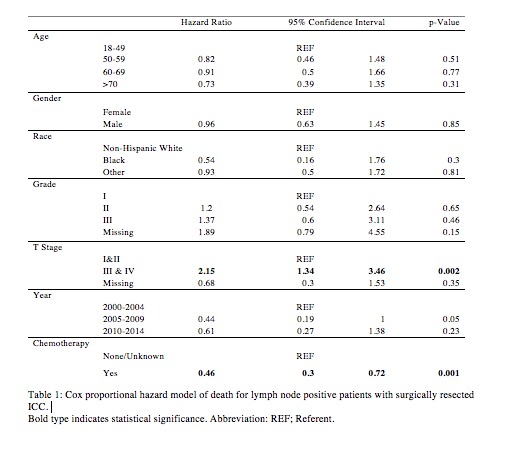
ADJUVANT CHEMOTHERAPY FOR INTRAHEPATIC CHOLANGIOCARCINOMA: APPROACHING CLINICAL PRACTICE CONSENSUS? Ariella M. Altman*, Scott Kizy, Schelomo Marmor, Adam Sheka, Jane Yuet Ching Hui, Todd Tuttle, Eric H. Jensen, Jason W. Denbo Department of Surgery, University of Minnesota, Minneapolis, MN Background: No randomized trial exists defining the role of adjuvant chemotherapy in patients with resected intrahepatic cholangiocarcinoma (ICC). Retrospective studies suggest adjuvant chemotherapy may improve survival for select patients, yet treatment guidelines remain poorly defined. We sought to describe the utilization and role of adjuvant chemotherapy in patients with resected ICC. Methods: An augmented version of the SEER database was used to identify patients with resected ICC from 2000-2014. Patients with metastatic disease or those who received chemoradiation as first-line therapy were excluded. Patients were grouped by date of diagnosis (2000-2004, 2005-2009, 2010-2014), T, and N stage. Multivariable logistic regression models were utilized to identify predictors of chemotherapy use for each of the time-periods. Kaplan-Meier curves and Cox proportional hazard models were used to identify survival trends. Results: We identified 1,223 patients who underwent surgical resection for ICC - 194 diagnosed from 2000-2004, 379 from 2005-2009, and 650 from 2010-2014. Patient, tumor, and treatment characteristics were similar between groups. However, the use of chemotherapy increased over time, from 33% to 37% to 41% in each respective time period, (p<.05). Receipt of chemotherapy increased in lymph node positive patients (32% in 2000-2004, 57% in 2005-2009, and 60% in 2010-2014; p<.05) and patients with T3/T4 tumors (40% in 2005-2009 to 60% in 2010-2014; p≤.01) over time, but not in patients with lymph node negative or T1/T2 disease (Figure 1). No predictors were identified upon evaluation of factors associated with chemotherapy use from 2000-2004. However, from 2005-2009, lymph node positivity was significantly associated with increased chemotherapy use, while increasing age and male sex were associated with decreased use (p<.05). From 2010-2014, significant predictors of chemotherapy use were lymph node positivity and T3/T4 tumors, while increasing age and male sex were associated with decreased use (p<.05). Median overall survival across the three periods (2000-2004, 2005-2009, and 2010-2014) was 32, 32, and 41 months, respectively (p=0.06). After adjusting for patient factors, chemotherapy use was significantly associated with a decreased hazard ratio of death among lymph node positive patients (p<.05, Table 1). ). Stage T3/T4 disease was associated with a significantly increased hazard ratio of death. (p≤0.05, Table 1). Conclusion: The use of chemotherapy in patients with surgically resected ICC has evolved over the last 15 years. The majority of patients with T3/4 tumors or node-positive disease are now receiving chemotherapy. Increased utilization of chemotherapy in patients with advanced T stage and lymph node positive disease, may in part explain the improvements seen in overall survival for surgically resected ICC. 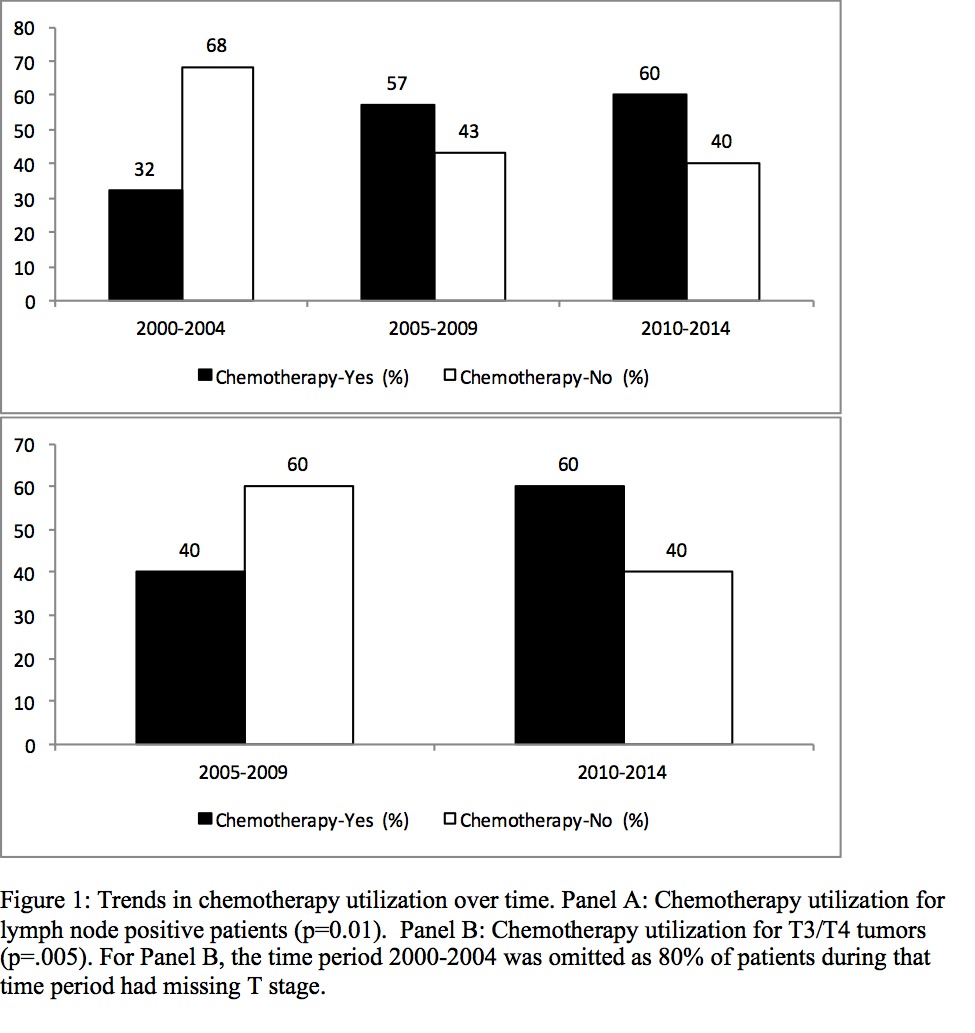
Figure 1: Trends in chemotherapy utilization over time. Panel A: Chemotherapy utilization for lymph node positive patients (p=0.01). Panel B: Chemotherapy utilization for T3/T4 tumors (p=.005). For Panel B, the time period 2000-2004 was omitted as 80% of patients during that time period had missing T stage. Back to 2018 Posters |
|||||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.