|
Back to 2018 Posters
DETOURS ON THE ROAD TO RECOVERY: WHAT FACTORS LEAD TO DELAY IN THE RETURN TO ONCOLOGIC THERAPY AFTER LIVER RESECTION?
Heather A. Lillemoe*, Rebecca K. Marcus, Bradford J. Kim, Nisha Narula, Catherine H. Davis, Thomas Aloia
Surgical Oncology, MD Anderson Cancer Center, Houston, TX
Objective: To determine perioperative factors associated with delayed return to intended oncologic treatment (RIOT) after liver resection.
Background: Poor recovery after cancer surgery delays RIOT and shortens cancer-specific survivals.
Methods: Consecutive patients undergoing hepatectomy from 2015-2017 were analyzed. 93% of cases were performed for malignancy. Pre- and post-operative factors, as well as perioperative outcomes, were compared between patients who had early (defined as ≤28 postoperative days) vs. delayed (>28 postoperative days) surgeon-determined clearance to RIOT. Univariate and multivariate analyses were performed using binary logistic regression and a backwards stepwise variable elimination method.
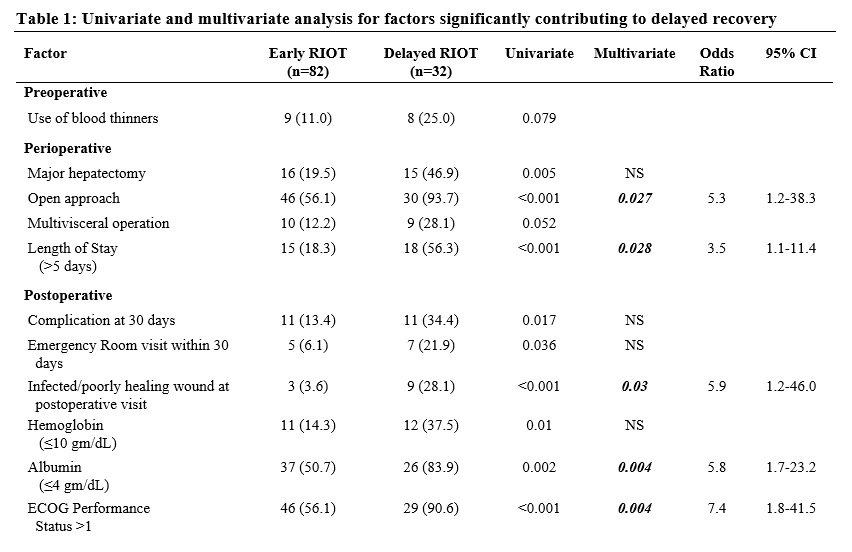
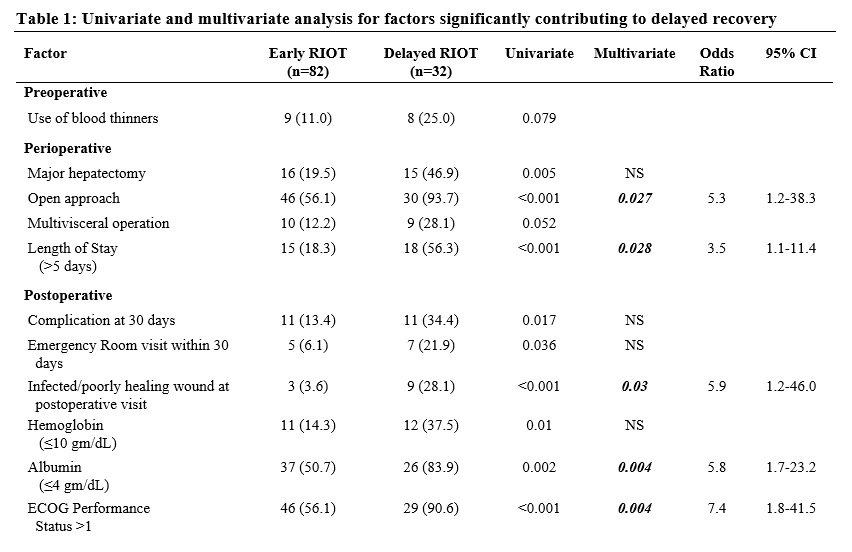
Results: Of 114 patients, 82 patients (72%) had early RIOT and 32 patients (28%) had delayed RIOT. Relevant perioperative factors including gender, BMI, age, and receipt of preoperative chemotherapy were comparable between the groups. The only preoperative factor associated with delayed RIOT was the use of blood thinners. Operative factors associated with delayed RIOT included major hepatectomy, combined multivisceral procedure, and open surgical approach. Postoperatively, longer length of stay (LOS), the occurrence of any complication, and emergency room visit were associated with delayed RIOT. In addition, at the first postoperative visit, the presence of an infected/poorly-healing wound, Eastern Cooperative Oncology Group (ECOG) performance status >1, and lower hemoglobin and albumin levels were associated with longer RIOT (Table 1). On multivariate analysis, independent predictors of delayed RIOT were open approach (OR 5.3), longer LOS (OR 3.5), infected/poorly healing wound (OR 5.9), postoperative albumin level ≤ 4gm/dL (OR 5.8), and poor postoperative performance status (OR 7.4).
Conclusions: After hepatectomy for malignancy, return to necessary oncologic treatment has a substantial impact on survival. While many factors that affect timely RIOT are not modifiable, such as surgical approach or extent of resection, this analysis suggests that the avoidance of postoperative wound complications, including poor healing related to malnutrition, is crucial. To improve oncologic outcomes for liver surgery patients, surgeons should continue to focus on implementing the available best practices around this metric.
Back to 2018 Posters
|