|
TRANSVERSUS ABDOMINIS PLANE BLOCK REDUCES NARCOTIC USE AND PAIN AFTER ROBOT-ASSISTED DISTAL PANCREATECTOMY Monica A. Solis Velasco*2, Ana Sofia Ore2, Kathryn A. Stackhouse2, Koen Verkoulen2,1, Vimal Akhouri3, Mark P. Callery2, Tara S. Kent2, A. J. Moser2 1Surgery, Maastricht University Medical Center, Maastricht, Netherlands; 2Pancreas and Liver Institute, Beth Israel Deaconess Medical Center, Boston, MA; 3Anesthesiology, Beth Israel Deaconess Medical Center, Boston, MA
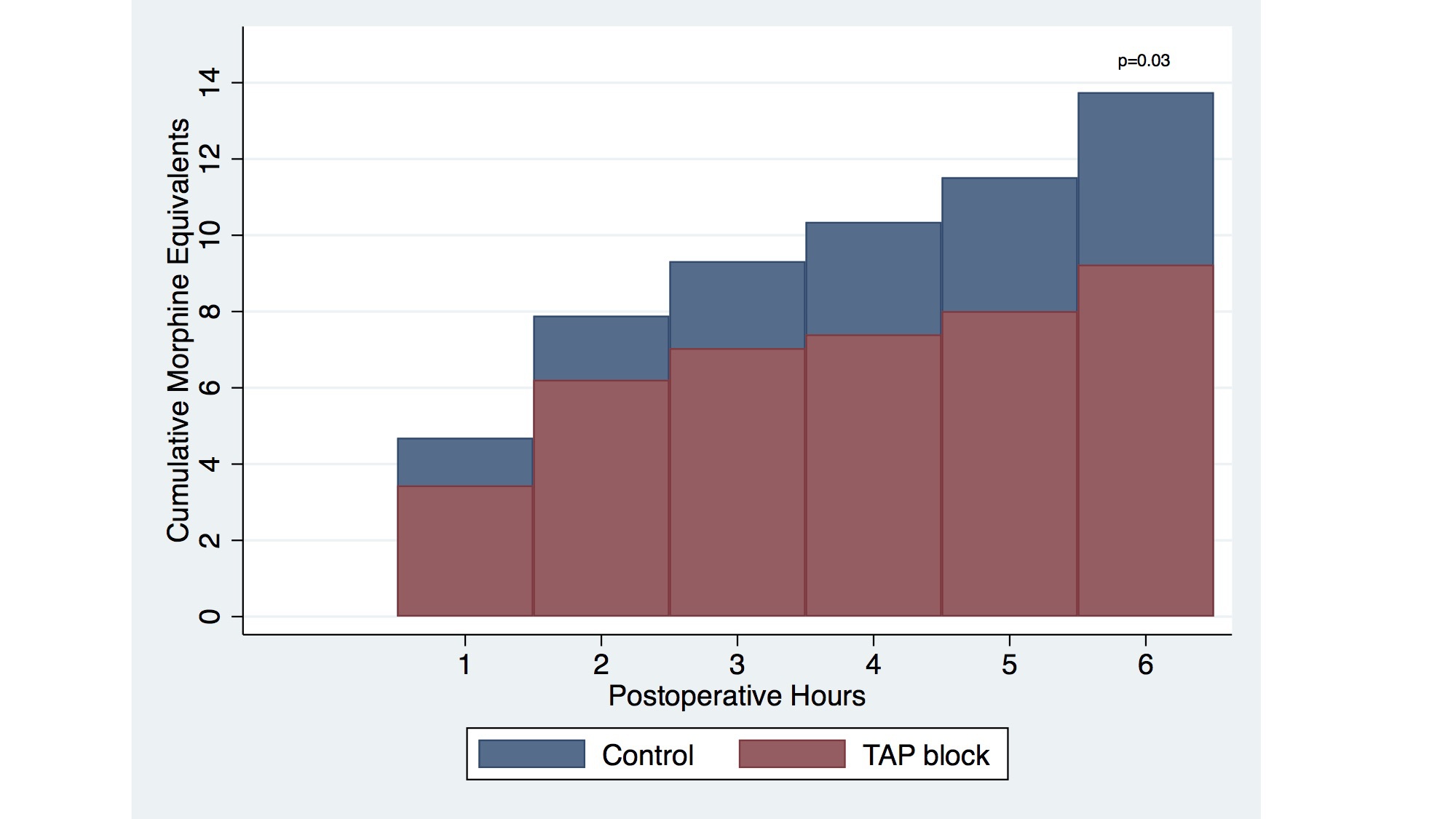
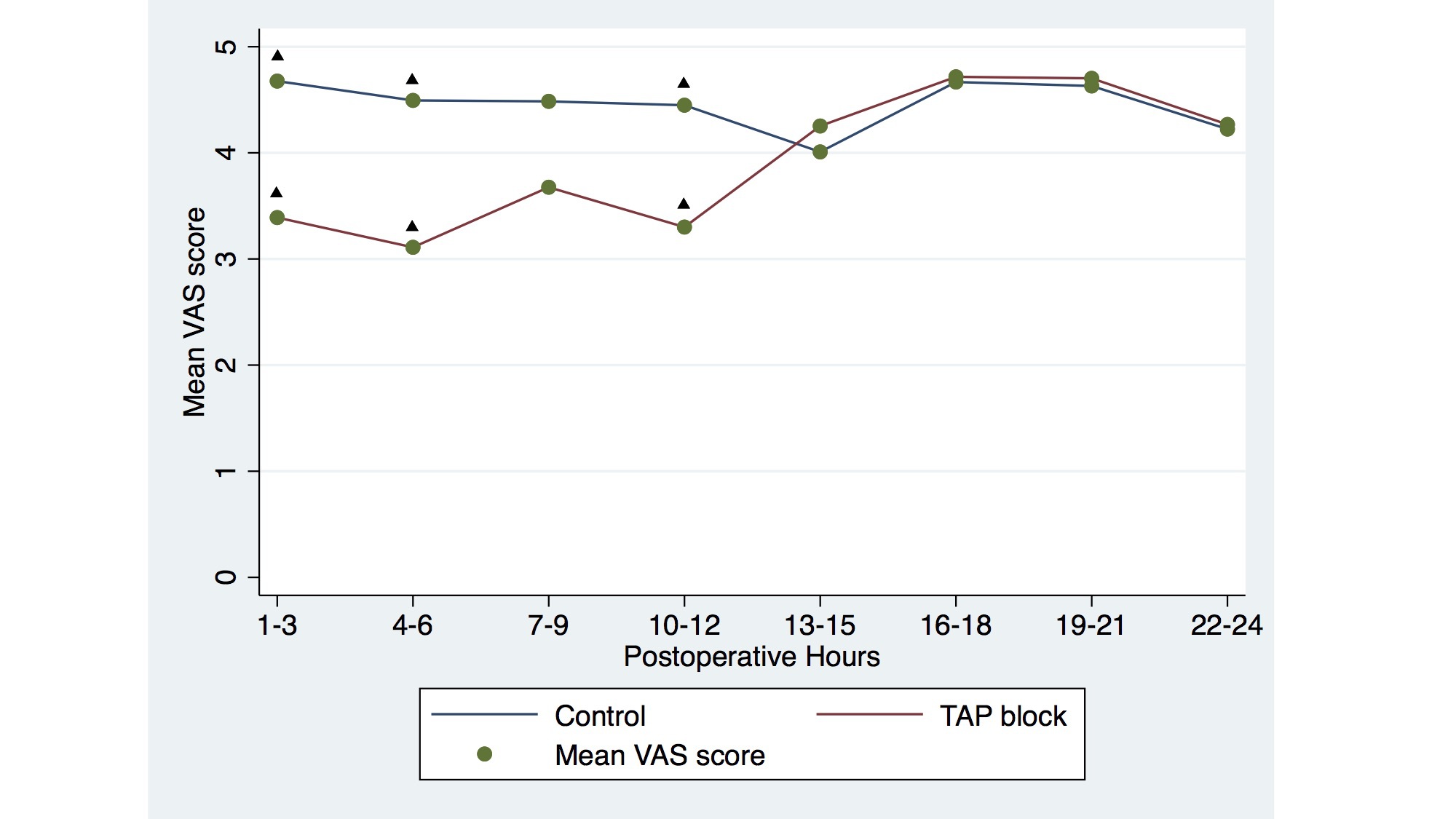
Background: Expediting postoperative recovery is a key objective of minimally-invasive distal pancreatectomy (DP) for pancreatic tumors. The effectiveness of transversus-abdominis plane (TAP) block at decreasing postoperative pain and opioid consumption after robot-assisted DP (RADP) is unknown. We hypothesized that TAP block reduces opioid administration and postoperative pain after elective RADP compared to standard multimodal analgesia alone. Methods: Retrospective cohort study of 81 patients undergoing RADP between June 2012 and October 2017. TAP block was used routinely after November 2015 (n=33). Bilateral laparoscopic-guided infusions of 60 mL 0.25% bupivacaine hydrochloride were performed at multiple levels. Given 4-8h bupivacaine duration, the primary outcome was cumulative opioid administration by postoperative hour six reported as intravenous (IV) morphine milligram equivalents (MME). Linear regression was used to analyze MME at 6 hours, adjusting for pre-specified variables. Secondary outcomes included average pain scores using the Visual Analogue Scale (VAS), length of stay (LOS), and 30-day comprehensive complication index (CCI). Results: The control and TAP groups had equivalent demographic and perioperative characteristics, including age, gender, body mass index, ASA score, age-adjusted Charlson comorbidity index, malignant disease, history of chronic pain, operation time, and estimated blood loss (EBL). Linear regression showed a significant association between IV MME and TAP block use (F[1,73] = 4.76, p=0.03). TAP patients consumed fewer MME than controls during the first six postoperative hours (β = -4.52, p=0.032) (Figure 1). The difference after adjusting for pre-specified variables was maintained independently of chronic pain history, operative time, and body mass index (β = -4.89, p=0.025). Mean VAS scores were significantly reduced after TAP block at six (3.22 ± 2.33 vs. 4.57 ± 2.08, p=0.009) and 12 hours (3.24 ± 1.94 vs. 4.45 ± 1.84, p=0.006), but not at 24 hours (3.88 ± 1.62 vs. 4.4 ± 1.58, p=0.129) (Figure 2). No significant differences in LOS (5 vs. 6 days, p=0.42) or 30-day CCI (20.9 vs. 12.2, p=0.61) were observed. Conclusion: Laparoscopic bilateral TAP block is associated with significantly decreased opioid consumption for 6 hours after RADP. Visual analogue pain scores were significantly reduced for the first 12 hours but did not affect hospital length of stay. Longer-acting TAP agents may significantly improve these results. Back to 2018 Posters |
|||||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.