|
Back to 2018 Posters
UTILIZATION OF NEOADJUVANT THERAPY IN GASTROINTESTINAL STROMAL TUMORS OF THE STOMACH: ANALYSIS OF THE 2006-2013 NATIONAL CANCER DATA BASE
Kevin M. Turner*2, Cara J. Joyce2, Jennifer L. Gnerlich1
1Surgery, LSU Health Sciences Center, New Orleans, LA; 2Loyola Stritch School of Medicine, Maywood, IL
Introduction: Neoadjuvant tyrosine kinase inhibitor (TKI) therapy has been shown to reduce tumor burden and improve survival in both primary and recurrent gastrointestinal stromal tumors (GIST) in recent institutional studies. However, no clear guidelines exist on optimal patient selection for neoadjuvant treatment. Our aim was to analyze factors associated with receipt of neoadjuvant therapy for gastric GISTs.
Methods: We conducted a retrospective, population-based cohort study of patients diagnosed with a gastric GIST and underwent surgery using the 2006-2013 National Cancer Data Base (NCDB) to examine clinical and pathological characteristics of patients treated with neoadjuvant therapy compared with adjuvant therapy. Unadjusted and adjusted odds ratios for patient demographics and clinical characteristics associated with neoadjuvant therapy were estimated from a multivariable mixed-effects logistic regression model with random intercepts to account for correlation within facilities.
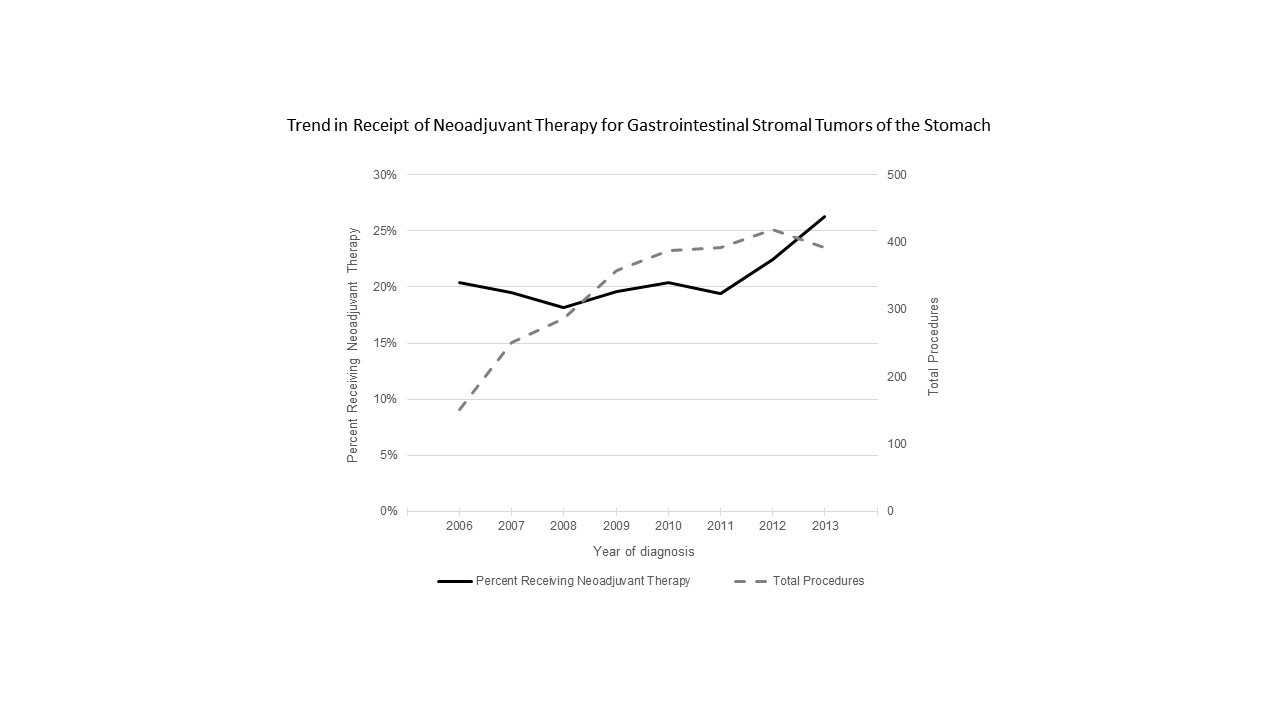
Results: Of the 2,638 patients with a gastric GIST who received systemic therapy, 554 (21.0%) received neoadjuvant therapy and 2,084 (79.0%) received adjuvant therapy. Use of neoadjuvant therapy increased over the study period (20.4% in 2006 vs. 26.3% in 2013, p<0.05). Patients who were more likely to receive neoadjuvant therapy had a Charlson-Deyo score of 0, were treated at an academic/research program, diagnosed in later years (2012-2013), had a tumor size of >10cm, or diagnosed with clinical Stage IV disease (p<0.05 for each) compared with those who underwent adjuvant therapy. While a majority of the study group received a partial gastrectomy 1,659 (63.7%), receipt of neoadjuvant therapy was associated with more extensive surgeries, notably gastrectomy with en bloc resection of an adjacent organ (p<0.001). After adjustment, patients receiving neoadjuvant therapy were significantly more likely to be treated in an academic/research program (aOR: 2.28, 95% CI: 1.29-4.03), have tumors > 10cm (aOR: 2.77, 95% CI: 1.91-4.03), diagnosed as clinical Stage IV (aOR: 2.31, 95% CI: 1.38-3.85), treated with near-total/total gastrectomy (aOR: 2.17, 95% CI: 1.01-4.65) or gastrectomy with esophageal resection (aOR: 1.98, 95% CI: 1.08-3.61). Neoadjuvant therapy was not associated with a difference in surgical margin positivity rates, length of stay, readmission rates, 30-day mortality rates, or overall survival when compared with adjuvant therapy.
Conclusion: Neoadjuvant therapy for the treatment of gastric GISTs has been increasingly utilized in clinical practice, particularly in a certain subset of patients. Even though patients receiving neoadjuvant therapy had poor clinical features, outcomes were similar to those receiving adjuvant therapy. More studies are required to determine the ideal therapeutic sequence for patients with gastric GIST.
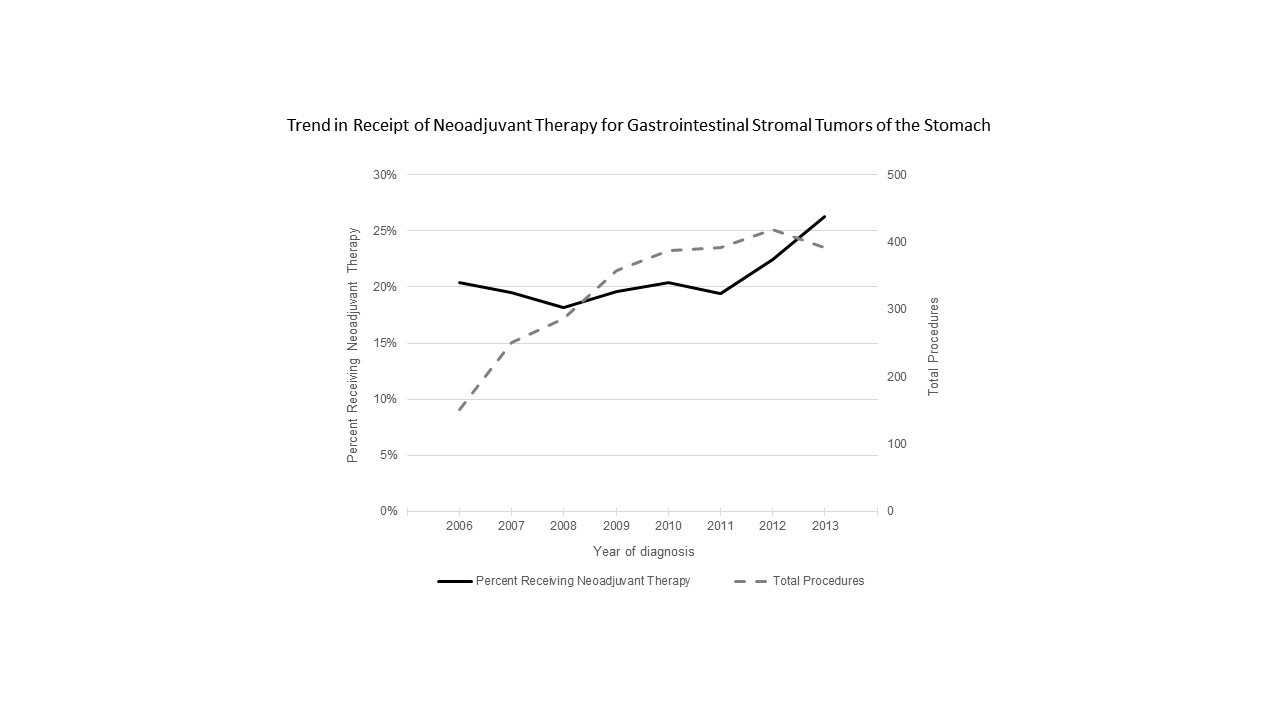
Trend in Receipt of Neoadjuvant Therapy for Gastrointestinal Stromal Tumors of the Stomach
Back to 2018 Posters
|