|
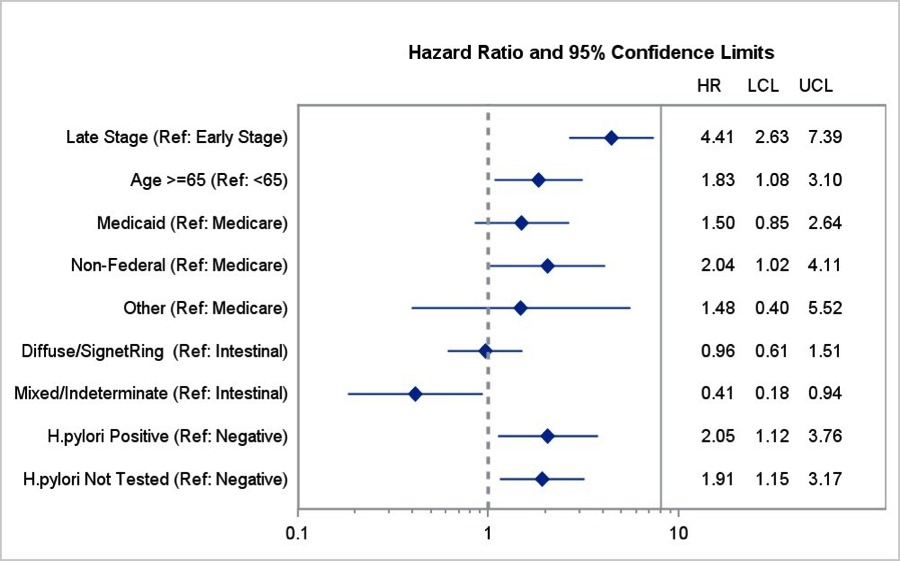
PRESENTATION AND SURVIVAL OF GASTRIC CANCER PATIENTS AT AN URBAN ACADEMIC SAFETY NET HOSPITAL Ryan Morgan*, Michael Cassidy, Susanna W. de Geus, Jennifer Tseng, David McAneny, Teviah Sachs Department of Surgery, Boston Medical Center, Boston, MA Introduction Gastric cancer (GC) incidence and mortality have steadily decreased in the United States, and yet GC remains a global health concern. In developing countries, GC accounts for more deaths than any other malignancy, except for lung and liver cancer. Due to multiple factors, immigrants with GC may experience worse outcomes relative to those born in the United States. We evaluated GC patient characteristics at an inner-city, safety-net hospital that serves a substantial immigrant and underserved patient population. Methods Demographics, tumor characteristics, comorbidities, treatment, and survival were analyzed for all patients diagnosed with gastric adenocarcinoma at our institution between 1/01/2004 and 6/30/2017. Chi square analyses were performed to determine dependence of stage at presentation upon demographics. Univariate and multivariate survival analyses were performed with Kaplan-Meier and Cox regression analyses, respectively. Results We identified 249 patients who were predominantly male (61.8%) with a mean age of 65.5 years at presentation. 74.3% of patients were born outside the United States or Canada, most commonly in the Caribbean (n=70), Africa (n=27), and Central America or Mexico (n=26). Most patients were either black (40.2%) or Hispanic (24.1%) and insured through federal programs (71.4%). The majority of the cohort (52.2%) had late-stage (Stage III/IV) disease. Over half of patients underwent surgical resection (51.0%), and 59.8% received chemotherapy and/or radiation. Hispanic race, Central American or Mexican birthplace, Medicaid insurance, and zip code poverty >20% were associated with later-stage presentation (all p<0.05). Late-stage presentation was associated with lower estimated median survival (75.0 vs 15.0 months, p<0.001). Residence in zip codes with >20% of the population in poverty was associated with decreased survival on univariate analysis (p<0.05) [Figure 1]. On multivariate analysis, increased hazard ratio for death was associated with late-stage presentation (HR=4.41, p<0.001), age ≥65 (1.83, p=0.018), non-federal insurance (2.04, p=0.045), and H. pylori infection (2.05, p=0.036); Decreased hazard ratio for death was observed for mixed/indeterminate histology (0.412, p=0.034) [Figure 2]. Conclusion This cohort of mostly immigrant patients with GC presented predominantly with late-stage disease. Hispanic race, Central American or Mexican birthplace, Medicaid insurance, and increased neighborhood poverty were associated with late-stage presentation. Higher neighborhood poverty was associated with decreased survival as well. On multivariate analysis, survival was negatively associated with late-stage presentation, increased age, H. pylori infection, and non-federal insurance. These factors merit further analysis to determine the value of screening strategies for gastric cancer in at-risk populations. 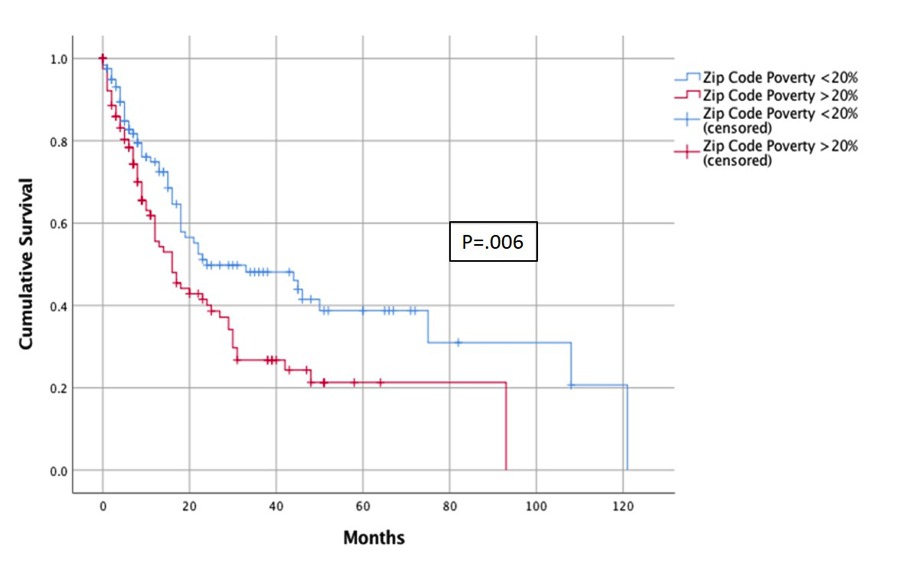
Figure 1: Survival of patients with Gastric Cancer based on zip code based poverty level Back to 2018 Posters |
|||||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.