|
 |
Back to 2018 Posters
TREATMENT BURDEN OF GASTRECTOMY AFTER NEOADJUVANT CHEMOTHERAPY FOR LOCALLY ADVANCED GASTRIC CANCER: A NATIONAL CANCER DATABASE ANALYSIS
Ana Sofia Ore*1, Monica A. Solis Velasco1, Kathryn A. Stackhouse1, Koen Verkoulen1,2, Andrea Bullock3, Jonathan F. Critchlow4, A. J. Moser1
1Institute of Hepatobiliary & Pancreatic Surgery, Beth Israel Deaconess Medical Center, Brookline, MA; 2Department of Surgery, Maastricht University Medical Center, Maastricht, Netherlands; 3Department of Hematology Oncology, Beth Israel Deaconess Medical Center, Boston, MA; 4Department of General Surgery, Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Neoadjuvant chemotherapy is increasingly used for gastric cancer and does not adversely impact gastrectomy outcomes or length of hospital stay. While minimally invasive gastrectomy is superior to open for early gastric cancer, comparative effectiveness data are lacking in the setting of locally-advanced gastric cancer (LAGC) following preoperative treatment. Considering recent data, we tested our hypothesis that minimally-invasive total/near total gastrectomy for LAGC does not adversely impact oncological outcomes compared to open after neoadjuvant chemotherapy and may reduce cumulative treatment burden in a large national cohort study.
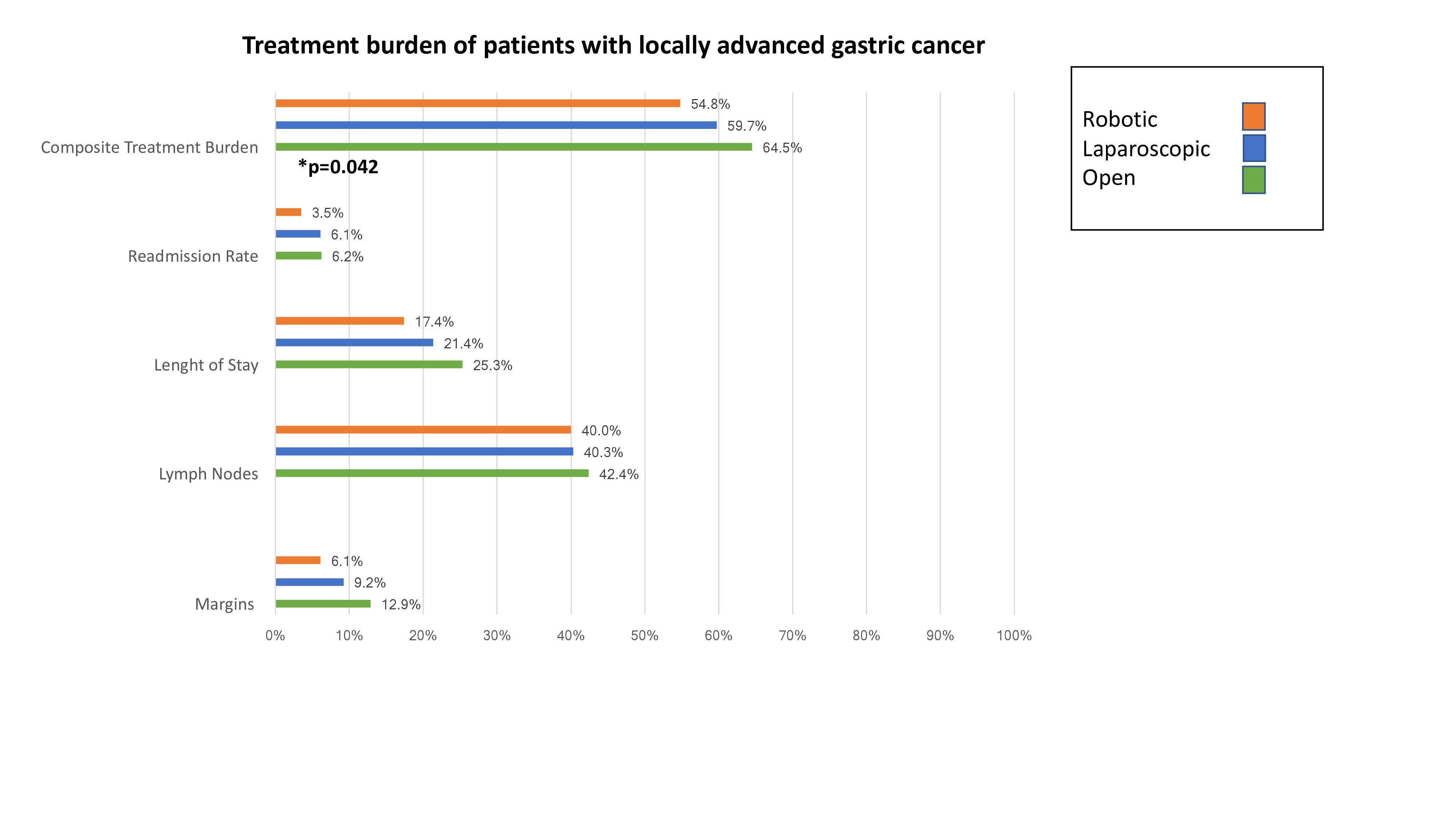
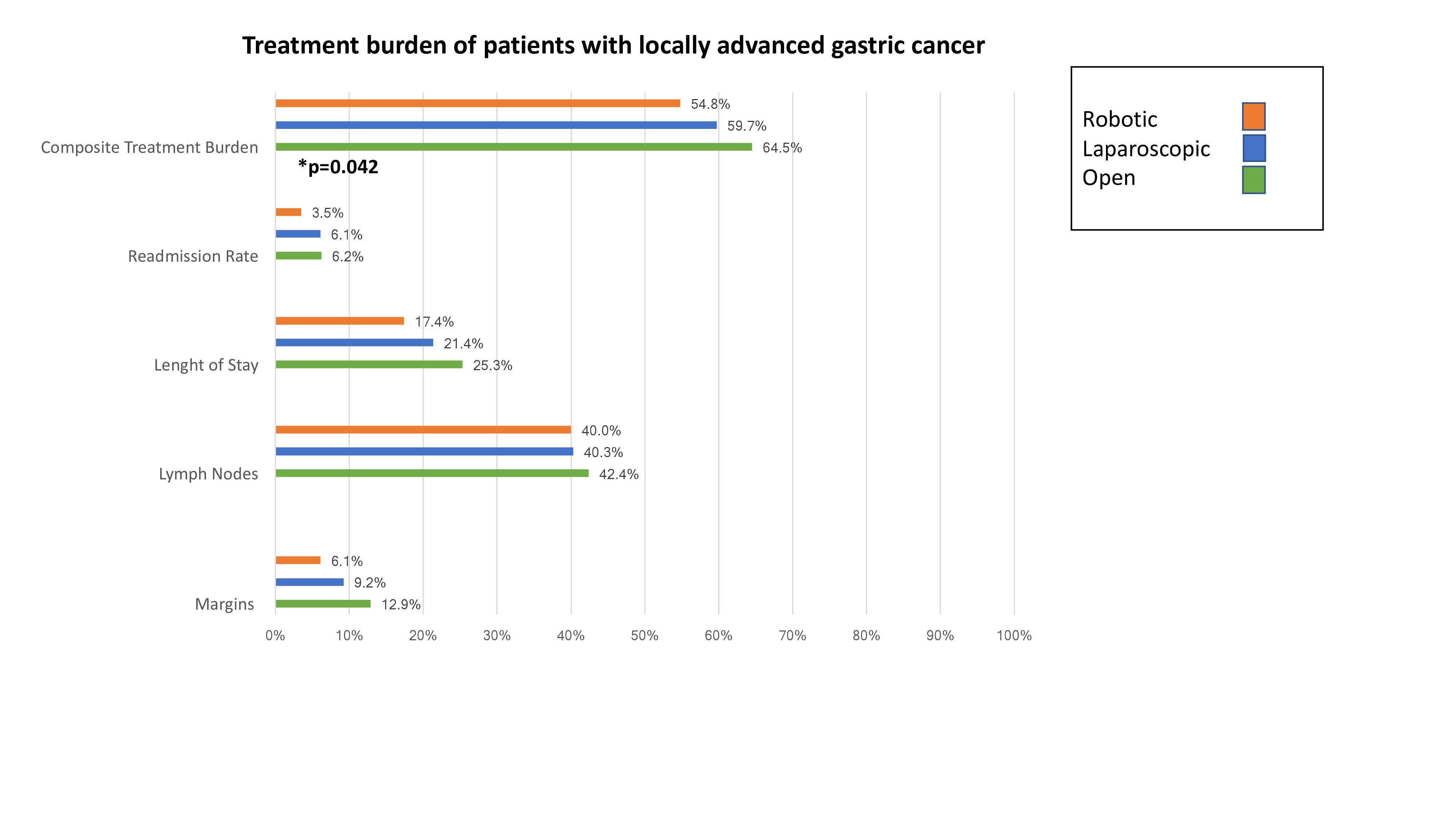
Methods: The National Cancer Database was queried to identify patients with LAGC (clinical AJCC T3-4N0, TanyN1) who underwent neoadjuvant chemotherapy followed by gastrectomy. Patients with unknown stage, treatment modality and/or treatment sequence were excluded. The primary outcome was treatment burden, a composite metric of database variables indicating one or more of the following adverse outcomes: positive resection margin, fewer than 16 resected lymph nodes, length of stay exceeding the 75th percentile for the cohort, and unplanned readmission within 30-days.
Results: 1716 patients underwent total or near total gastrectomy after neoadjuvant chemotherapy for LAGC between 2010-2015. Preoperative age, gender, race, and Charlson comorbidity scores were equivalent in all three groups. The only observed selection bias toward surgical approach was treatment in an academic center. 1189 patients (69.3%) underwent an open or unspecified resection, whereas 530 (30.7%) underwent either a laparoscopic (415, 24.0%) or robotic (115, 6.7%) approach. The laparoscopic approach experienced a 21.3% conversion rate compared to 10.4% during robotic. 64.5% of patients in the open cohort experienced a negative composite outcome compared to 59.7% in the laparoscopic and 54.8% in the robotic groups (p=0.042) Similarly, 90-day mortality was 6.7%, 4.2%, and 2.4% for the open, laparoscopic, and robotic groups, respectively.
Conclusion: Current NCDB outcomes do not indicate inferior oncological or surgical outcomes following minimally-invasive total or near total gastrectomy after neoadjuvant therapy for LAGC. Randomized clinical trials are needed to assess the effect size of surgical approach on treatment burden given selection bias observed between US centers participating in NCDB.
Back to 2018 Posters
|