
|
PERORAL ENDOSCOPIC MYOTOMY (POEM): A PROSPECTIVE CASE SERIES OF EIGHTY PATIENTS FOR TREATMENT OF ACHALASIA Aman B. Ali*, Vishwanath Chegireddy, Dmitry Zavlin, Joseph J. Nguyen-Lee, Nabil Tariq, Brian J. Dunkin General Surgery, Houston Methodist Hospital, Sugar Land, TX Background: Achalasia is an uncommon disease with an incidence of 1/100,000 people per year in the US. Peroral endoscopic myotomy (POEM) has been adopted by some as a less invasive alternative to laparoscopic esophago-gastric myotomy, but others have questioned its efficacy and the risk of post-operative gastroesophageal reflux disease. Objective: This study evaluated the safety and efficacy of POEM for the treatment of achalasia. Methods: This is a single center retrospective review of prospective data collected from the first 80 consecutive POEMs performed by a single experienced surgeon between September 2013 and November 2017. Patient demographics, procedure details, intraoperative and postoperative course, and symptom control were recorded. To assess efficacy, preoperative and postoperative Dysphagia Handicap Index (DHI) and Quality of Life in Reflux and Dyspepsia (QOLRAD) scores were obtained. Results: Table 1 reports the patient demographics and outcomes. Despite 40% (25/62) of patients having prior interventions for their achalasia, all 80 procedures were completed endoscopically with no conversions to laparoscopic, thoracoscopic, or open surgery. There were no serious postoperative complications such as delayed leak or bleed, and the median length of stay was 1 day. In addition, 77.5% of patients took no narcotics postoperatively. The postoperative dysphagia scores dropped significantly (DHI mean score 58.4 preop and 17.7 postop; p value < 0.001) and there was improvement in the average QOLRAD scores (4.4 preop and 6.6 postop; p value < 0.001)- indicating no significant development of gastroesophageal reflux after surgery. Conclusion: This single institution case series demonstrates that POEM is a safe and efficacious treatment alternative for achalasia even in patients with prior interventions. It is associated with almost no postoperative pain and results in significant resolution of dysphagia while not causing postoperative gastroesophageal reflux. 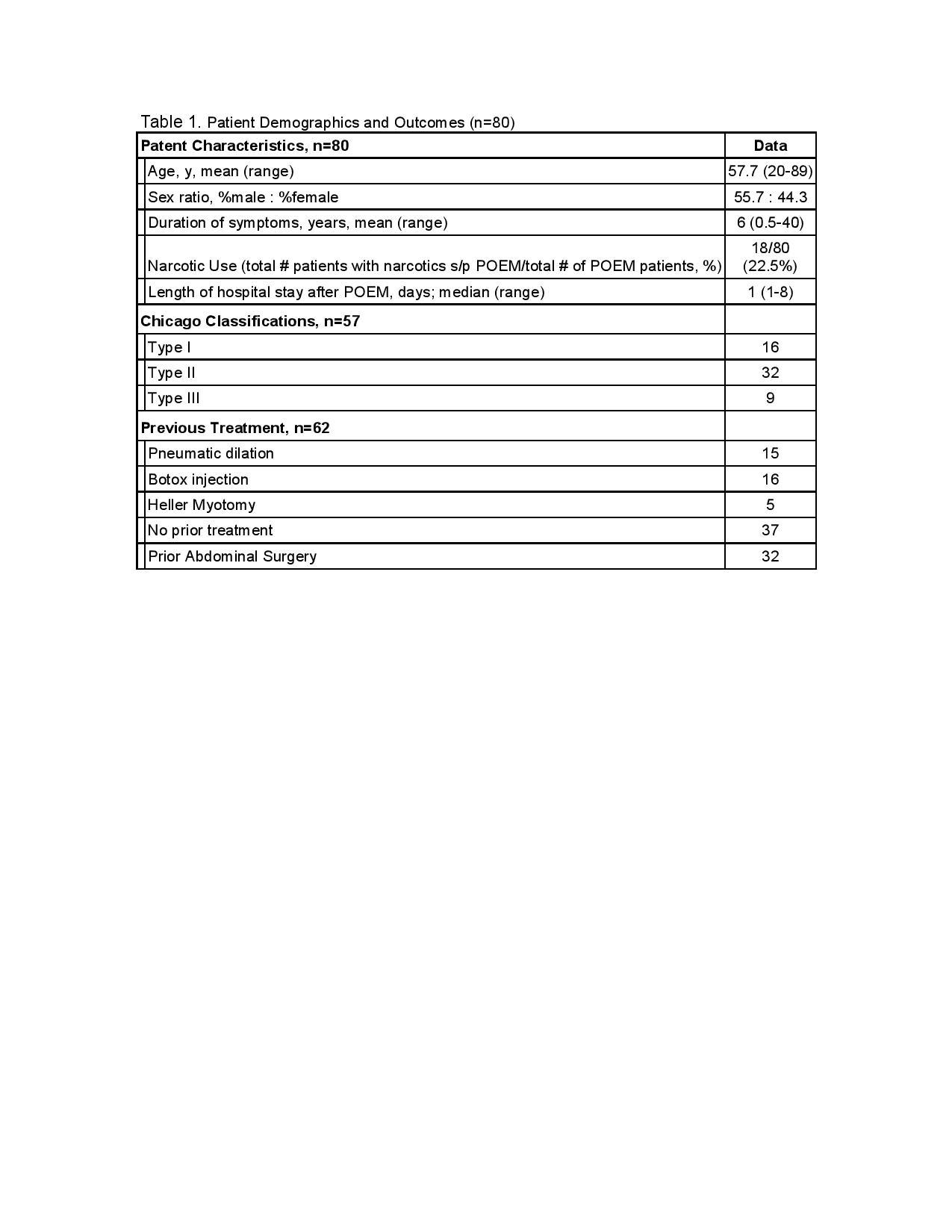
Table 1. Patient Demographics and Outcomes (n=80) Back to 2018 Posters |
|||||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.