|
 |
Back to 2018 Posters
LONG-TERM OUTCOMES IN PATIENTS REQUIRING ESOPHAGOSTOMIES DURING ESTABLISHMENT OF ESOPHAGEAL CONTINUITY
Wendy Jo Svetanoff*1, Kayla Hernandez3, Kathryn Davidson3, Thomas E. Hamilton1, Michael A. Manfredi2, Peter D. Ngo2, Charles J. Smithers1, Russell Jennings1
1Department of Surgery, Boston Children's Hospital, Brookline, MA; 2Department of Gastroenterology, Boston Children's Hospital, Boston, MA; 3Feeding and Swallowing Program, Boston Children's Hospital, Boston, MA
Introduction: Little is known about long-term outcomes in patients requiring an esophagostomy prior to restoration of esophageal continuity. Our aim was to look at the feasibility of maintaining the native esophagus, identify complications, and assess feeding ability following esophageal reconstruction.
Methods: A retrospective analysis (IRB # P00004344) of all patients who received an esophagostomy during restoration of esophageal continuity from 1993-2017 was performed. Analysis of outside hospital procedures, types of procedures performed, complications, and current eating ability was completed.
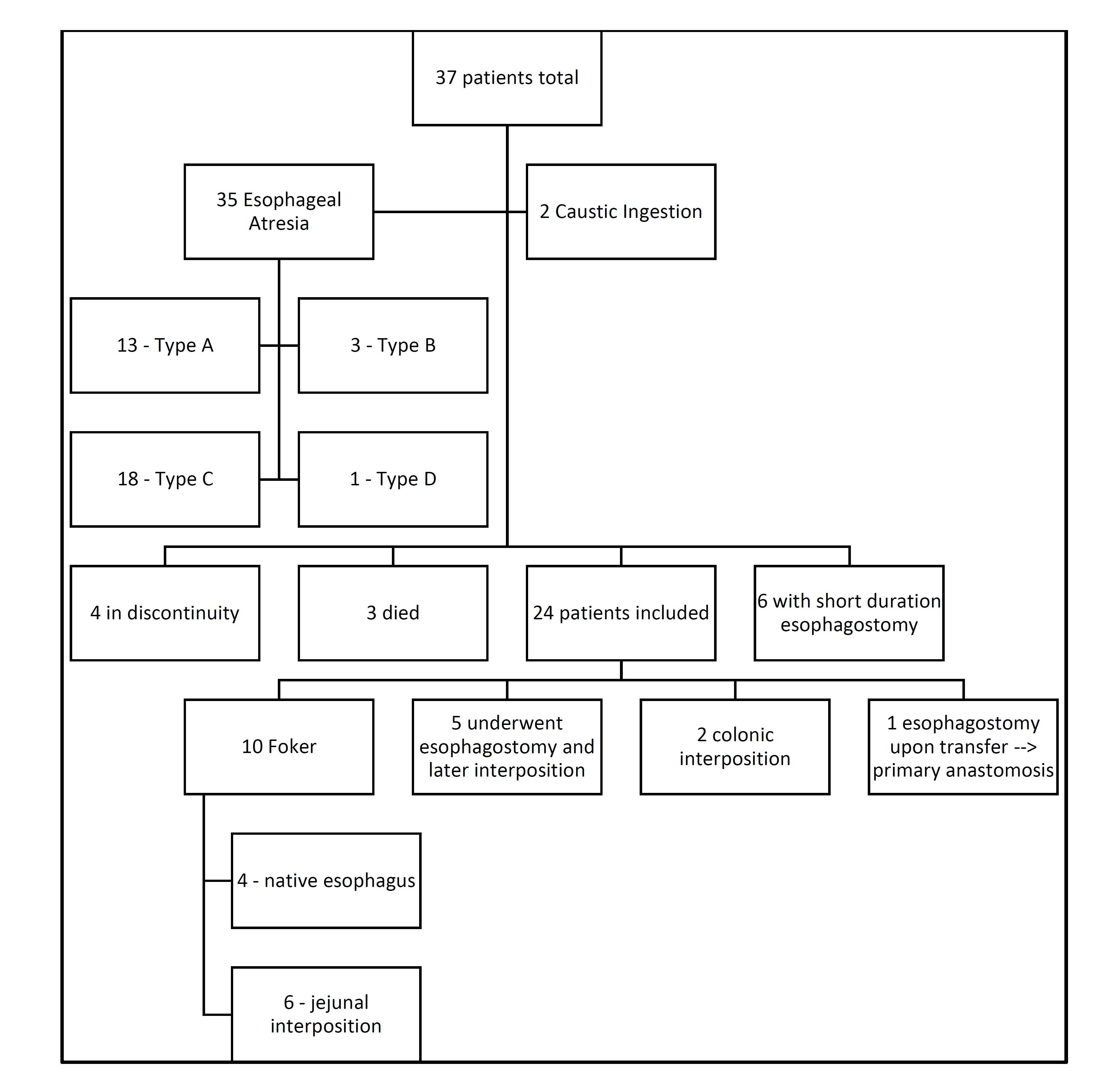
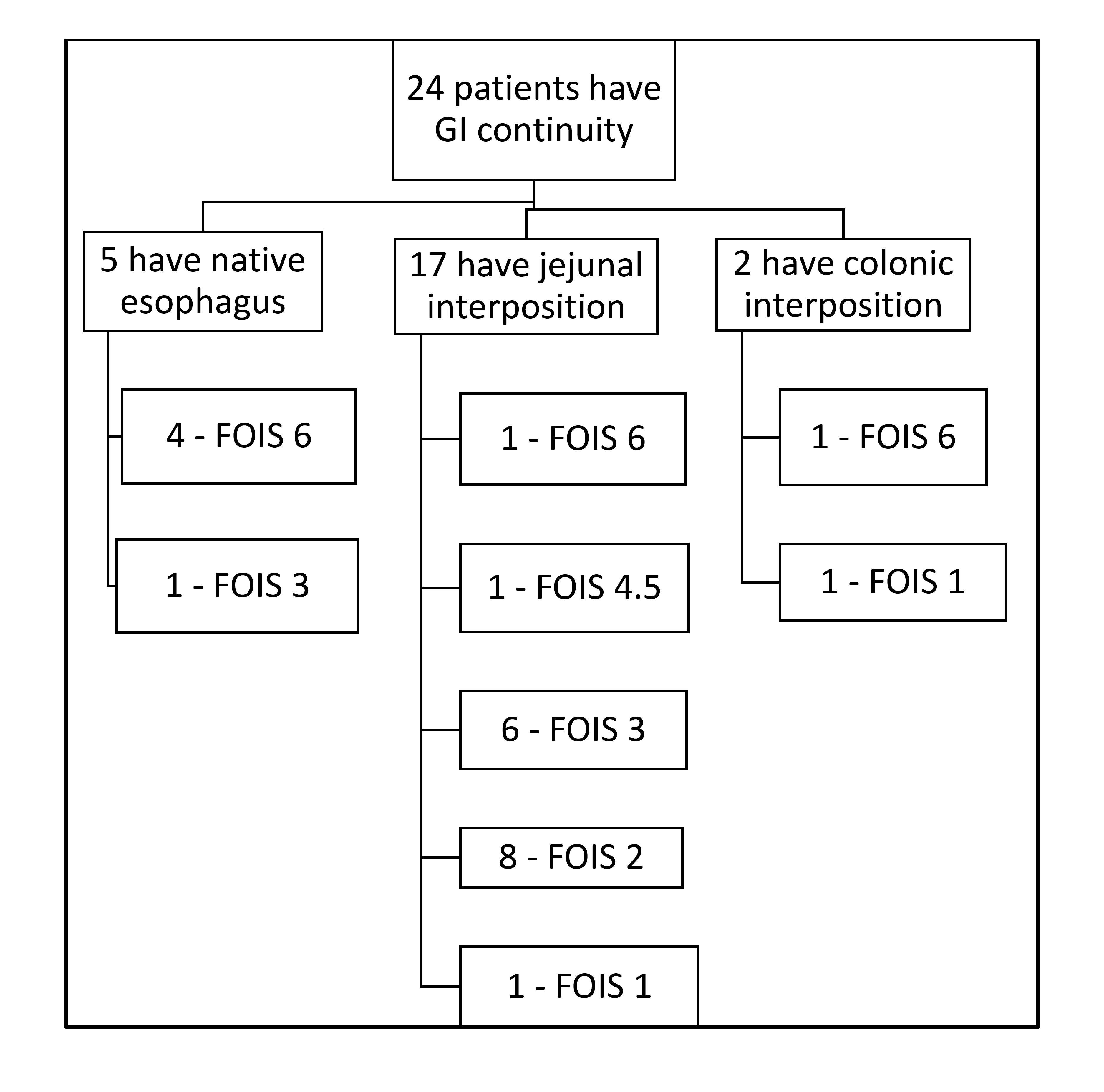
Results: Thirty-seven patients were identified, with 2 patients suffering a caustic ingestion and 35 with esophageal atresia (EA). Of the 13 patients excluded, 6 had a short duration esophagostomy as part of a staged interposition, 3 died prior to repair, and 4 are still in discontinuity (Figure 1). Fourteen patients had esophagostomies upon transfer, with 8 receiving an esophagostomy as their only operation. At our institution, 10 underwent the Foker process (FP) with 4 (40%) able to maintain their native esophagus. Seventeen patients received a jejunal interposition, 6 of whom had attempted a primary esophageal repair prior to the interposition. Six patients required > 8 surgeries before establishing definitive continuity; 5/6 had undergone FP, while only 2 were patients with an initial esophagostomy. Six patients had a jejunal interposition as the first operation after transfer; only one suffered a leak post-operatively. Fourteen patients in total developed an anastomotic leak, and 3 were also noted to have a chyle leak. Using the Pediatric Functional Oral Intake Score (FOIS), 6 patients scored a 6 on most recent evaluation (full oral intake), with 4 patients having their native esophagus; 1 scored a 4.5 (full oral with modified diet); 7 scored a 3 (consistent oral intake with tube feedings); and 8 scored a 2 (minimal oral intake with tube feeds). Of the patients still on tube feedings, 5 have had surgery to re-establish continuity in the past 6 months. For the 5 patients with a native esophagus, 4 are taking full meals, and 1 are FOIS 3 (Figure 2).
Conclusion: Although maintaining the native esophagus with FP is feasible, it is ideal in patients with a virgin esophagus and reasonable for those who received an esophagostomy as the initial operation. More recently we have been performing jejunal interpositions in patients with previous esophageal surgery; these patients have required less surgery and have lower leak rates. Once esophageal continuity has been established, 14/24 were able to take consistent oral intake (3+ FOIS score), with all but two taking some food orally. Patients with complex EA should be cared for at major esophageal centers to optimize outcomes, as an interposition may be the best option in those requiring an esophagostomy.
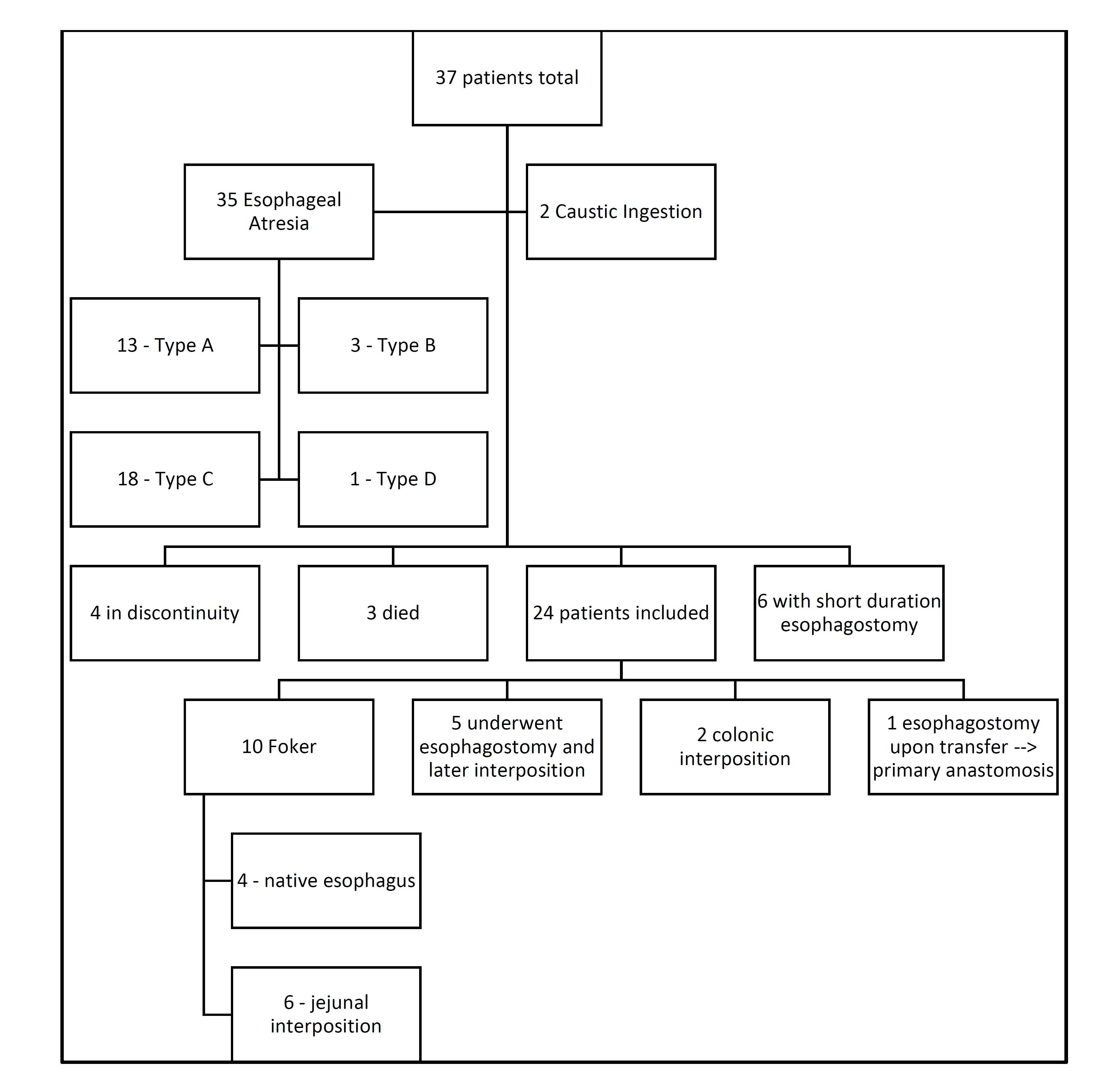
Figure 1: Patient Demographics. 37 patients were eligible for the review, and 24 were included. Both colonic interpositions were done prior to 2002. Surgeon preference switched from FP for native esophageal salvage to jejunal interposition in 2015.
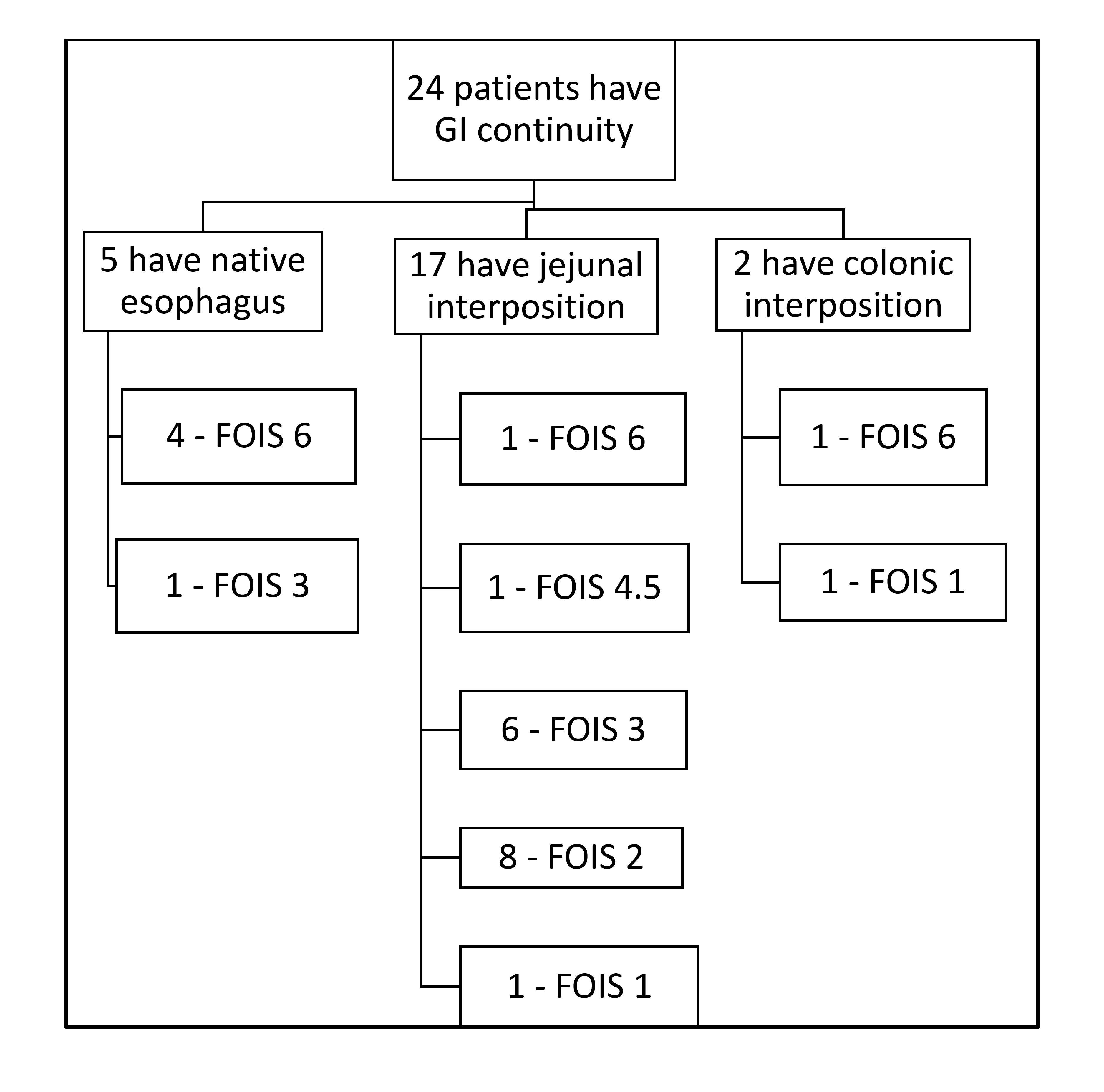
Figure 2: Post-Operative Feeding Ability. Of the patients able to retain their native esophagus, 4 underwent Foker process and 3 required at least 7 surgeries. Of those ultimately requiring a jejunal interposition, 5 have had surgeries in the past 6 months and are already taken some oral intake.
Back to 2018 Posters
|