|
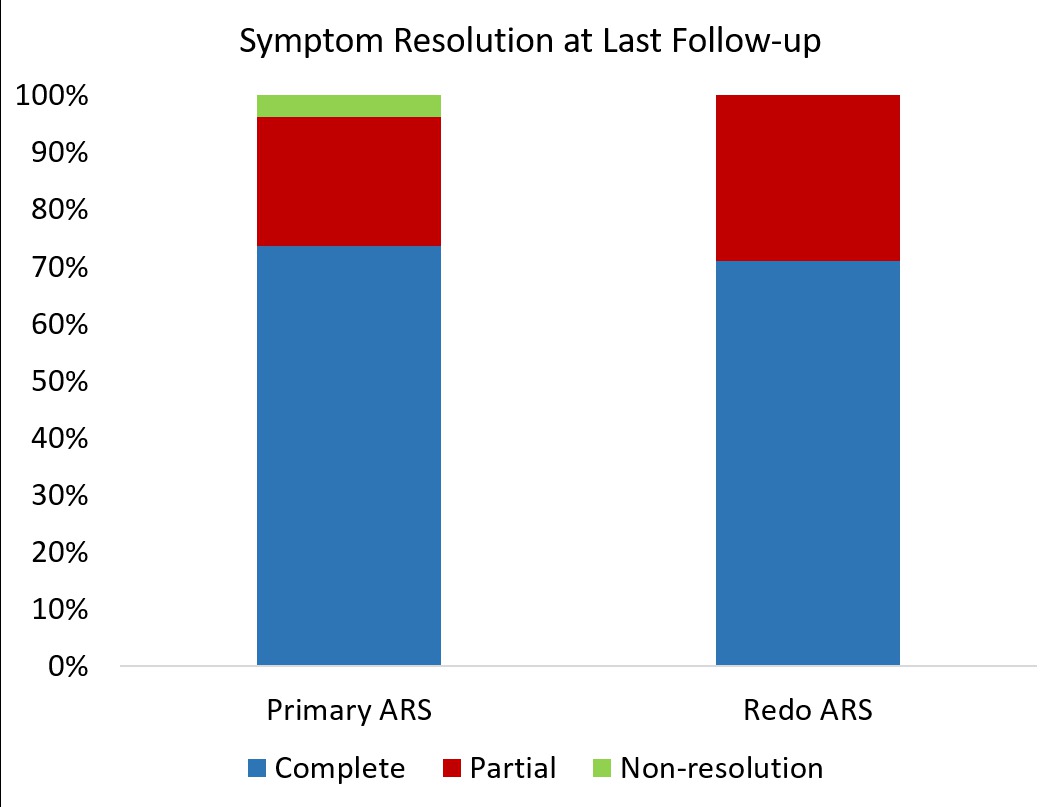
A CASE FOR THE ROBOT: COMPARING OUTCOMES OF ROBOTIC REOPERATIVE AND PRIMARY ANTIREFLUX SURGERY Adham Elmously*, Adriana Valera, Katherine D. Gray, Timothy Ullmann, Thomas J. Fahey, Cheguevera Afaneh, Rasa Zarnegar Surgery, New York Presbyterian Hospital - Weill Cornell Medicine, New York, NY Background: The role of robotic-assisted laparoscopy for anti-reflux surgery (ARS) is controversial. We aimed to determine the efficacy of robotic surgery in primary and reoperative ARS. Methods: A retrospective review of all patients undergoing primary or reoperative robotic ARS at a single tertiary referral center between 2012 and 2017 was performed. Patients undergoing paraesophageal or hiatal hernia repair and fundoplication were included. Demographics, perioperative outcomes, and long term follow up data were collected. Results: A total of 200 patients were included (168 primary ARS; 38 reoperative ARS). Seven (18.4%) of the reoperative patients had 2 or more prior foregut operations. Mean age was 54.5 ± 16.2 and 75% of patients were ASA 1 or 2, p > 0.05 between groups. A learning curve was constructed demonstrating that 70 cases are required to achieve proficiency, after which mean operative time was 121±17 minutes in primary procedures vs. 226 ± 12.8 minutes in the reoperative group (p<0.001) (Figure 1). There were no conversions to open and there was one intraoperative mucosal perforation in a reoperative case (1/38, 2.6%). Median length of stay was 22 hours, IQR 16 - 29 hours (21 hours in the primary group versus 24 hours in the reoperative group, p < 0.01). Thirty-five patients (18%, 30 primary and 4 reoperative) were discharged within 8 hours and 115 patients (58%) were discharged within 24 hours from operation. Readmission rate in this short-stay cohort was 4.3% (5/115). On multivariable regression, length of stay <24 hours was not a predictor of readmission (OR 1.0, CI 0.9 - 1.0, p = 0.30), however diabetes was an independent predictor of readmission (OR 5.0, CI 1.6-1.8, p=0.007). At a median follow up of 328 days (IQR 52-675), 6 (3%) patients required endoscopic dilations for dysphagia (4 primary and 2 reoperative, p= 0.4) and 9 (4.5%) patients required re-operative ARS. On last follow up, 97% of primary and 96.3% of reoperative patients had complete or partial resolution of symptoms (p=0.4) (Figure 2). Conclusion: In this large cohort of patients undergoing robotic ARS, we demonstrate equivalent clinical outcomes in primary and reoperative patients, while demonstrating that selected patients can be discharged home within 24 hours of operation with low rates of re-admission. 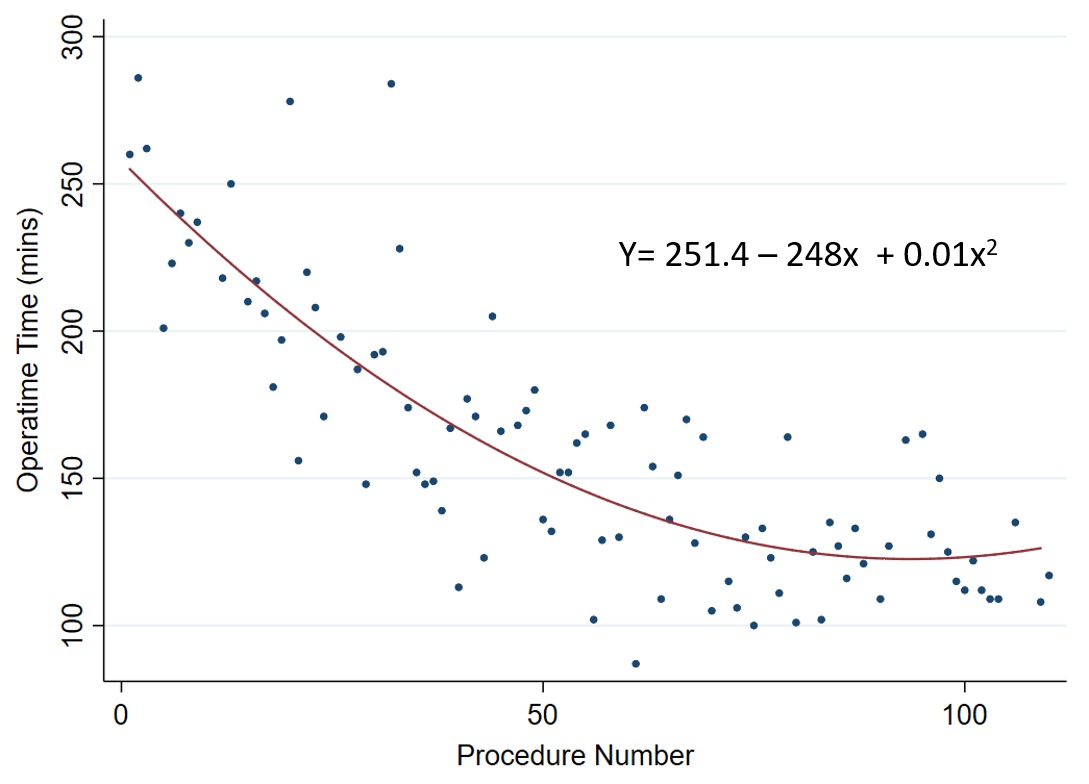
Figure 1. Learning curve for primary robotic anti-reflux surgery. Quadratic regression of operating time and sequential procedure number demonstrating proficiency at 70 cases. Back to 2018 Posters |
|||||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.