
|
PREVALENCE OF CHEST PAIN IN PATIENTS WITH ACHALASIA AFTER LAPAROSCOPIC HELLER MYOTOMY AND PARTIAL FUNDOPLICATION: LONG-TERM FOLLOW-UP. Angélica Rodríguez-Garcés*1, Fernanda Romero-Hernández1, Enrique Coss-Adame2, Miguel A. Valdovinos2, Janette Furuzawa-carballeda3, Daniel Azamar-Llamas3, Raul Chávez-Fernández3, Fidel López-Verdugo3, Gonzalo Torres-Villalobos1 1Experimental Surgery, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico city, Mexico; 2Gastroenterology, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico city, Mexico; 3Immunology and Rheumatology, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico city, Mexico
Introduction: Achalasia is a primary motor disorder of the esophagus characterized by aperistalsis of the esophageal body and incomplete relaxation of the lower esophageal sphincter (LES). The clinical features are dysphagia, weight loss, regurgitation and chest pain. Laparoscopic Heller Myotomy (LHM) improves all the above-mentioned symptoms significantly. However, chest pain can be cumbersome and in some cases, it may not be completely eliminated. Aim: To determine the prevalence of chest pain in patients with achalasia and evaluate the improvement after surgical treatment. Also, to identify if there is any variable that may be associated with the persistence of pain. Material and Methods: Prospective, randomized, clinical trial in which patients with diagnosis of idiopathic achalasia by esophagogram, upper endoscopy and high-resolution manometry (HRM) were included. Patients underwent LHM and partial fundoplication, Dor or Toupet. To evaluate the symptoms, Eckardt questionnaire was applied before and after surgery (1 month, 6, 12 and 24 months). PH-monitoring 6 months after surgery was performed in all patients. For the statistical analysis, the SPSS program was used (IMB SPSS Inc., Chicago IL, United States). Results: Eighty-two patients were included, mean age 40.82 (±14.60), 49 (59.8%) were women. The most frequent type of achalasia was type II (73.2%), followed by type I (24.4%) and type III (2.4%). Of these patients, 40 (48.8%) underwent Toupet fundoplication and 42 (51.2%) Dor. Regarding preoperative chest pain, 17.1% did not present pain, 39% had occasional pain, 8.5% daily, and 35.4% during each meal. One month after surgery, 58% had no pain, 35.8% occasionally, 3.7% daily, and 2.5% each meal. At 6 months, 58.6% had no pain, 37.1% occasionally and 4.8% each meal. At 12 months, 56.4% had no pain, 38.2% occasionally and 5.5% daily. Finally, at 24 months 51.3% had no pain, 41% occasionally, 5.1% daily and 2.6% each meal (Figure 1). According to the type of fundoplication, there was no statistical difference at the any point in the follow up (Table 1). For the 24 hr pH-monitoring 6 months after surgery, 80.7% of the patients with chest pain had a normal acid exposure. Conclusions: LHM with partial fundoplication improves chest pain significantly; however, in some cases it is not completely eliminated. Most of the patients with chest pain had a normal pH-study, these suggest that mechanism leading to residual chest pain after LHM in achalasia patients is not related to reflux and may have other explanations.
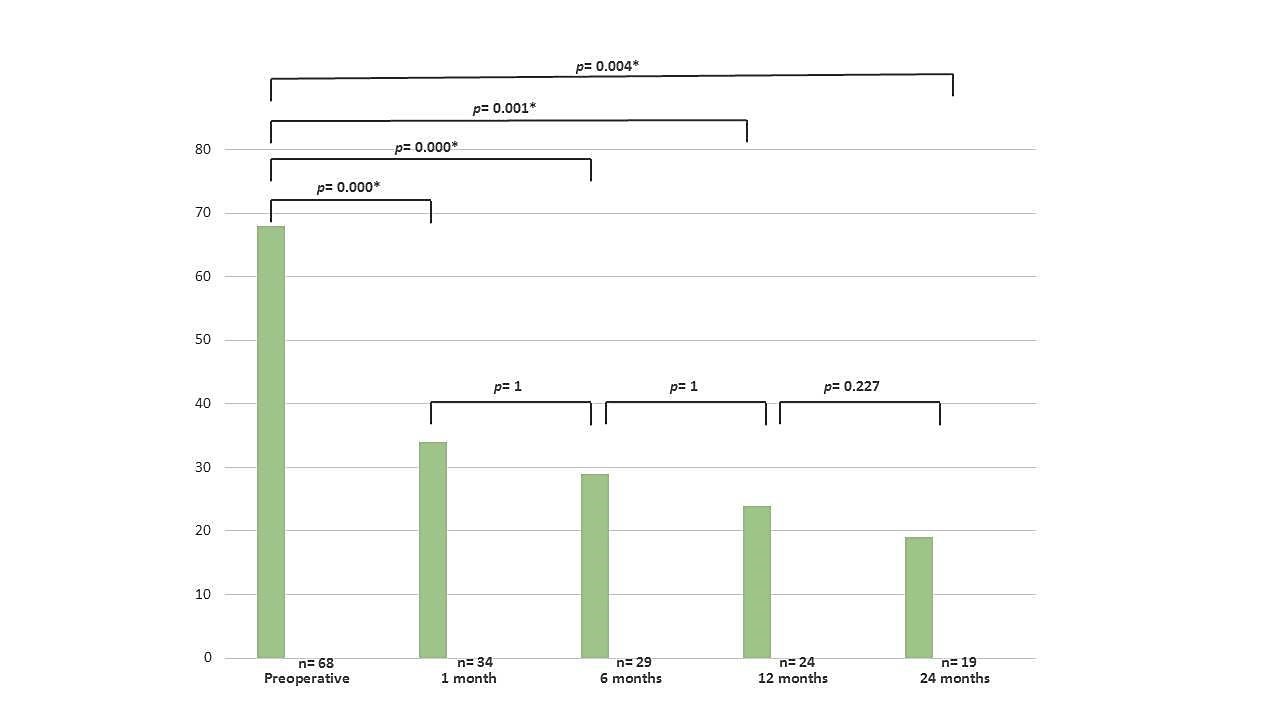 Figure 1. Preoperative and postoperative chest pain. Back to 2018 Posters |
|||||||||||||||||||||||||||||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.