|
 |
Back to 2018 Posters
THE ASSOCIATION OF BMI AND POSTOPERATIVE OUTCOMES AFTER ELECTIVE PARAESOPHAGEAL HERNIA REPAIR
Samuel Torres Landa*1, Jordana Cohen2, Chris Wirtalla1, Robert Caskey1, Andrew J. Sinnamon1, Veronica Zoghbi1, Robert A. Swendiman1, Ari D. Brooks1, Noel N. Williams1, Octavia Pickett-Blakely3, Daniel T. Dempsey1, Kristoffel Dumon1
1Gastrointestinal Surgery, Hospital of the University of Pennsylvania, Philadelphia, PA; 2Renal, electrolyte and hypertension division, Hospital of the University of Pennsylvania, Philadelphia, PA; 3Gastroenterology, Hospital of the University of Pennsylvania, Philadelphia, PA
Background: Current studies assessing the association of body mass index and postoperative outcomes after non-bariatric procedures are contradictory. Some studies have reported that obese patients are at higher risk for postoperative outcomes. However, other studies have shown a protective effect ("Obesity Paradox") as BMI increases. This association has not been clarified in elective paraesophageal hernia repairs.
Aim: Assess the association between body mass index and 30-day surgical outcomes in elective paraesophageal hernia repairs.
Methods: We conducted a retrospective analysis using the National Surgical Quality Improvement Program (NISQIP) dataset from 2005 to 2015. Patients who had laparoscopic, open, or transthoracic elective paraesophageal repair were included. Patients were divided into four BMI groups: < 18.5, 18.5 - 24.99, 25 - 29.99, and > 30. Univariate analysis was performed. Logistic regression was also used to determine the association between BMI class and surgical outcomes (mortality, readmission, reoperation, and complications) with adjustment for potential confounders.
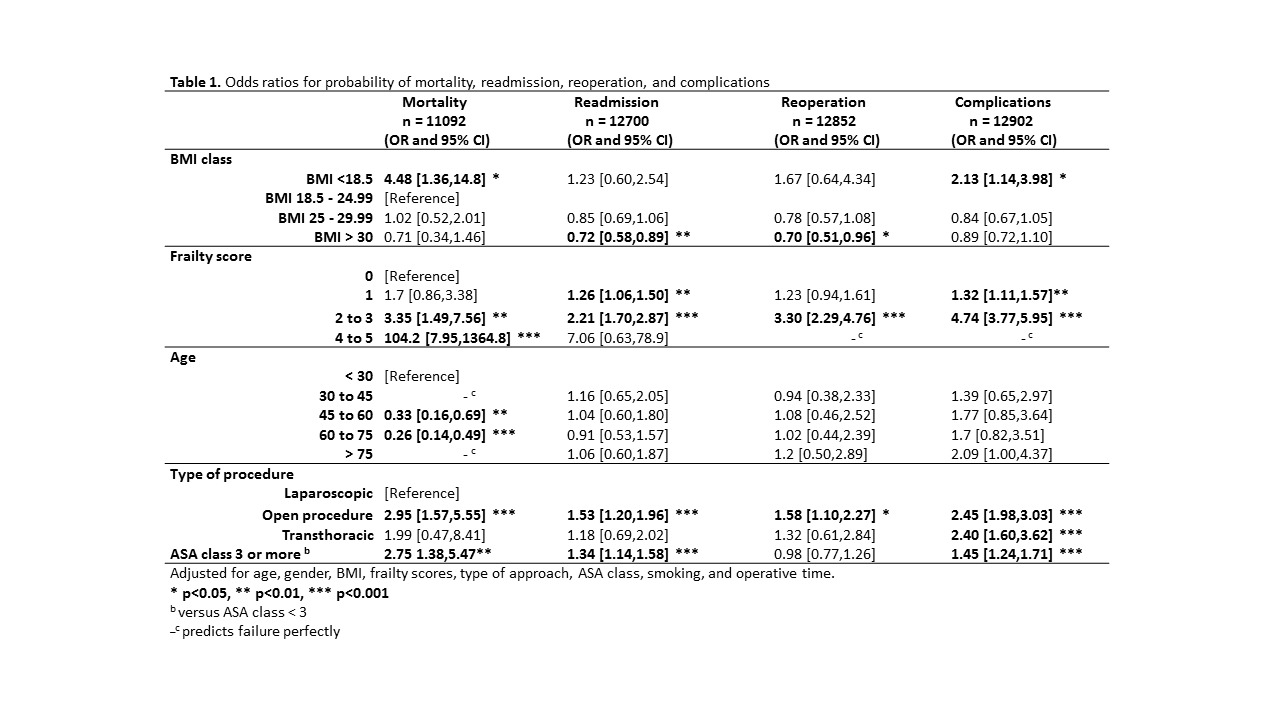
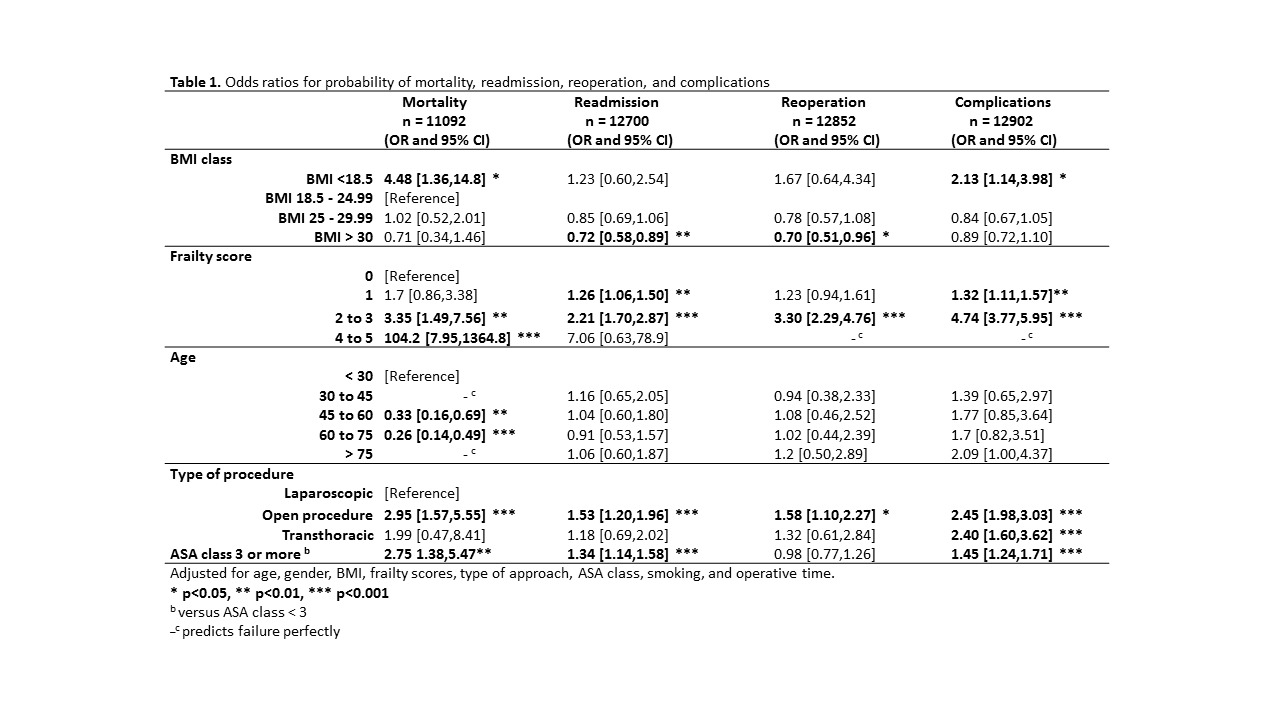
Results: A total of 13,283 patients met inclusion criteria, with a mean age of 61.1 (±14.2). Of these, 71.5% were women. Laparoscopic procedure type represented 91.3%, followed by open (7.0%), and transthoracic (1.7%). Across each successive BMI group, significant univariate differences were found in age, race, gender, type of procedure, frailty score, smoking status, and ASA class (p < 0.05). In multivariable logistic regression models using normal BMI as the reference group, underweight was associated with an increased 30-day mortality (OR = 4.48, p = > 0.05) and complication rates (OR = 2.13, p = > 0.05). Obesity was associated with a decreased risk for readmission (OR = 0.72, p = > 0.01) and reoperation rates (OR = 0.70, p = > 0.05). Frailty scores of 2 and 3, as well as open procedures were associated with significant increased odds of mortality, readmission, reoperation, and complication rates (Table 1).
Conclusion: Obesity seems to be related with a protective effect for readmission and reoperation, but not for mortality and complication rates in elective paraesophageal hernia repairs. Underweight patients are associated with an increased risk for mortality and complication, but not for readmission nor reoperation rates. The reason for these phenomena is yet to be elucidated.
Back to 2018 Posters
|