|
Back to 2018 Posters
LAPAROSCOPIC TRANSHIATAL ESOPHAGECTOMY FOR INVASIVE ESOPHAGEAL ADENOCARCINOMA.
Walaa F. Abdelmoaty*1, Christy M. Dunst2
1Providence Portland Medical Center, Tigard, OR; 2GMIS, The Oregon Clinic, Portland, OR
INTRODUCTION:
The technique and application of the laparoscopic total esophagectomy has evolved since we reported the first series in 1997. At that time, its role in invasive cancer treatment was unknown. Over the past twenty years distal esophageal adenocarcinoma has become the primary indication for esophagectomy and the use of neoadjuvant chemoradiotherapy (nCRT) become standard of care. These changes have occurred simultaneously with the expansion of minimally invasive surgery. The aim of this study is to report the modern experience with laparoscopic transhiatal esophagectomy (LTHE) for invasive adenocarcinoma.
METHODS:
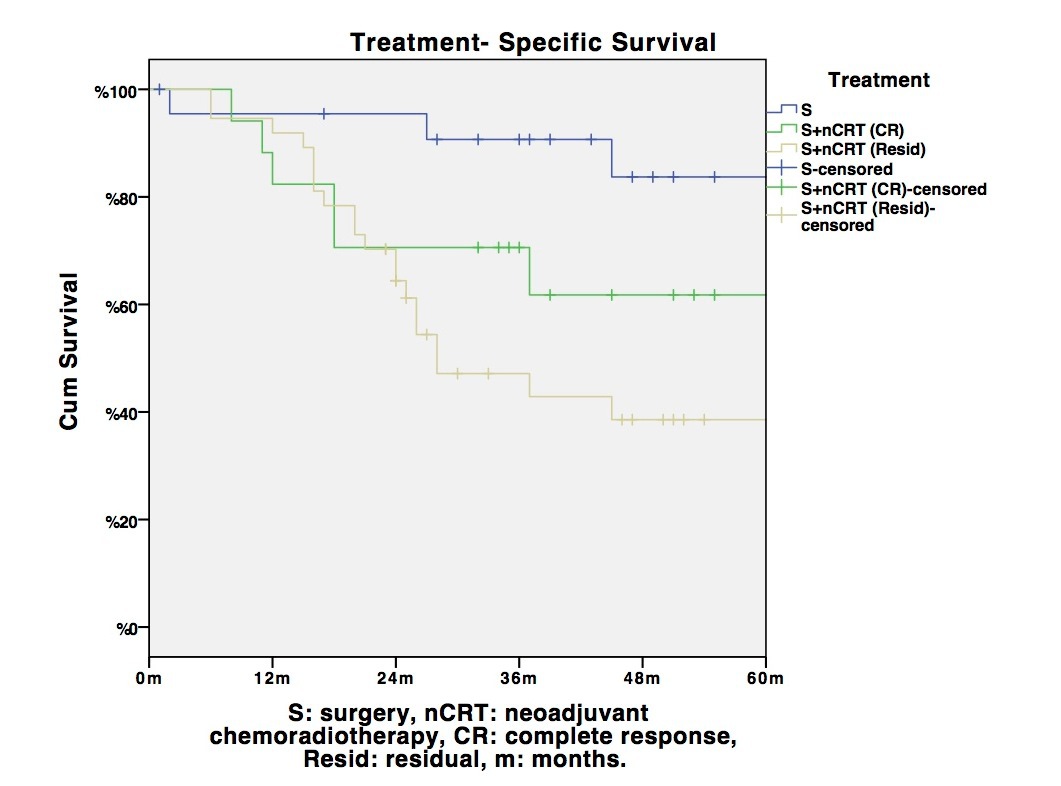
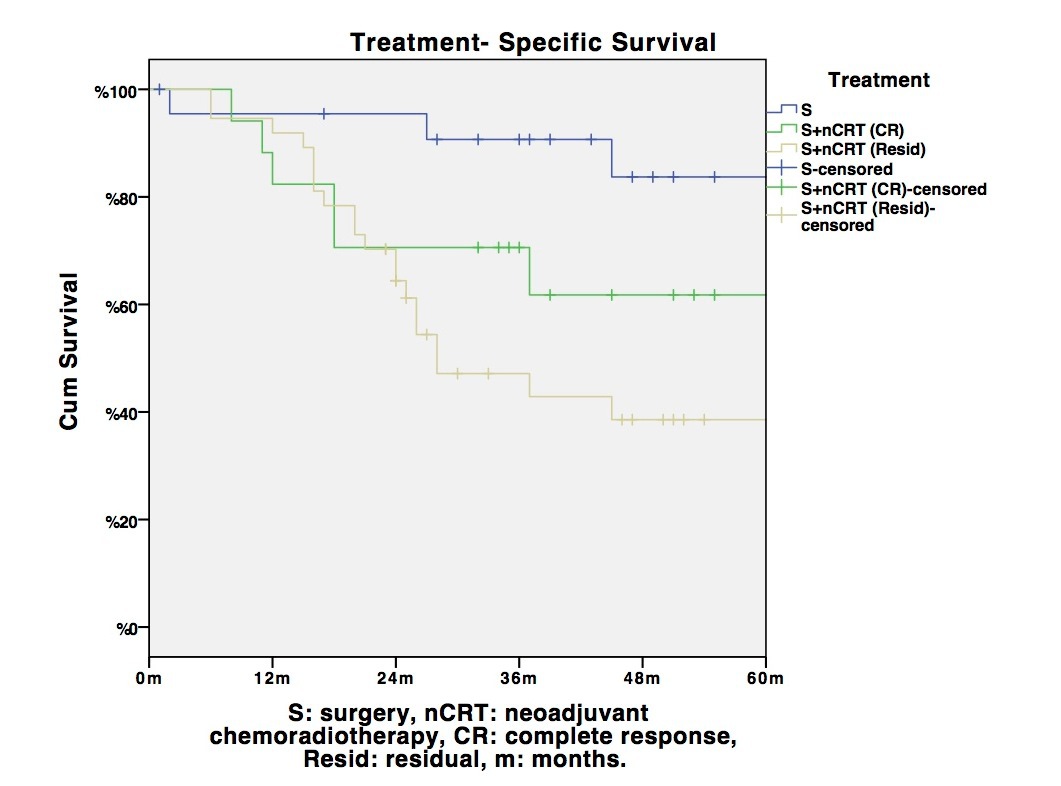
All patients who underwent LTHE between 2007 and 2016 were reviewed after IRB approval. A total of 91 patients were identified; 9 were excluded (1 squamous cell carcinoma, 2 refractory high grade dysplasia, 4 end stage motility disorder, 1 GIST, 1 recalcitrant stricture). All remaining patients had extended celiac and lower mediastinal lymph node dissection. Complications were categorized according to the Clavien-Dindo classification. Anastomotic leaks were further analyzed for severity. Survival rates were calculated with Kaplan-Meier curves.
RESULTS:
Eighty-two patients (13 women and 69 men) had LTHE for invasive adenocarcinoma. The mean age was 68 years (45-91) and mean BMI 27.81 (16.02-47.08). All tumors were located in the distal esophagus/proximal stomach (39% Siewert I, 57% Siewert II, 4% Siewert III). Twenty one patients (26%) were clinical stage I, 26 (32%) stage II, 35 (42%) stage III. nCRT was given to 56 patients (68%). Conversion to open was 6%.
The final cohort, of patients who had their esophagectomy completed laparoscopically, included 77 patients. Mean blood loss was 128 ml and median length of stay was 12 days. The median lymph node harvest was 19. Overall complication rate was 45% (50 complications in 35 patients: 6 grade I, 22 grade II, 12 grade IIIb, 8 grade IVa). Ninety day mortality was 4%. Anastomotic leak rate was 22%. None of the leaks required revision, takedown, or more than an endoscopic procedure.
Overall 5-year survival was 48%: disease-specific 58%. The 5-year survival for patients treated primarily with surgery is 83%, whereas for patients with a complete pathologic response to nCRT was 62% compared with 39% for those with residual disease.
CONCLUSION:
Laparoscopic transhiatal esophagectomy clearly has a role in current esophageal cancer treatment and can be performed with curative intent in patients with distal esophageal/proximal gastric tumors. The increased mediastinal visibility and a modern focus on oncologic principles seem to have a positive impact on cancer survival compared to the open transhiatal approach.
Back to 2018 Posters
|