|
 |
Back to 2018 Program and Abstracts
SALVAGE MINIMALLY INVASIVE SURGERY AFTER FAILED INITIAL PERCUTANEOUS DRAINAGE AS STEP-UP APPROACH IN PANCREATIC NECROSIS: RESULTS OF A PROSPECTIVE STUDY
Aditya Kulkarni*1, Rajesh Gupta1, Surinder S. Rana3, Mandeep Kang2, Harjeet Singh1, Vishal Sharma3, Madhu Khullar4
1Division of Surgical Gastroenterology, PGIMER, Chandigarh, Chandigarh, India; 2Radiology, PGIMER, Chandigarh, India; 3Gastroenterology, PGIMER, Chandigarh, India; 4Experimental Medicine, PGIMER, Chandigarh, India
Introduction: In our experience, the use of percutaneous drainage (PCD) in infected pancreatic necrosis led to improved outcomes and obviated the need for surgery in a significant proportion. However, prolonged use of PCD has a possibility of developing simmering sepsis, gradual nutritional depletion, and late-onset organ failure. Hence, the timing of switching from PCD to surgical intervention becomes important. We aimed to ascertain the optimal timing of intervention with video-assisted retroperitoneal debridement (VARD) and to look at mortality and morbidity in infected pancreatic necrosis managed with the two approaches.
Methodology: This prospective study was conducted from July 2016 to November 2017. Patients with moderately severe and severe acute pancreatitis (revised Atlanta) who failed to improve or deteriorated within 7 days after PCD were included. Patients who did not respond to aggressive PCD management received minimally invasive surgical intervention. Primary endpoints included mortality, morbidity, and requirement of surgery.
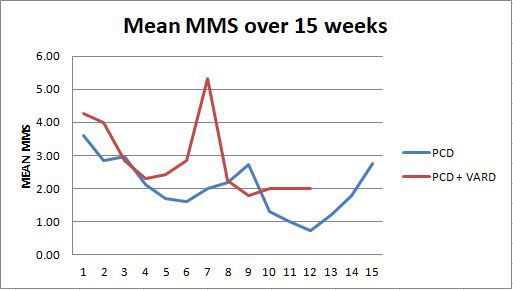
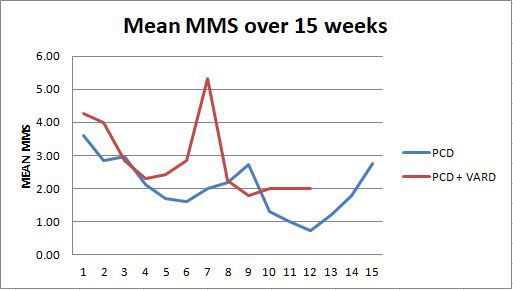
Results: 55 patients were assessed and 36 were included. Predominant etiology was alcohol (61%). Severe acute pancreatitis was present in 88.9% (n=32). Mean APACHE and modified Marshall Score (MMS) scores at presentation were 10.3± 5.5 and 3.69±2.6 respectively. MCTSI at time of presentation was 8.72±1.66. Both groups were comparable in terms of demographic data, APACHE II score, MMS score, MCTSI score at first CT, and incidence of infected necrosis. Overall, 63% (35/55) patients were successfully managed with PCDs alone. In those who failed initial PCD drainage, the PCD success rate was 44% (16/36). Indications for surgery included unresolved sepsis in 7 patients and colonic ischemia, bowel obstruction and flank abscess in one each. 3 patients developed PCD-related entero-cutaneous fistulae and were successfully managed conservatively. 8 surgical interventions were performed in 7 patients (VARD-6, minimal incision-2). Two patients required open necrosectomy for bowel obstruction and colonic ischemia. Patients were operated at a mean of 48.2 ±6.6 days from onset of pain. Mean MMS remained similar between the two arms for the first 4 weeks of illness; thereafter surgery arm had higher mean MMS scores, which were significantly higher at 7 weeks of illness (p=0.05) (Image 1). The incidence of positive blood culture (p=0.03) and requirement of parenteral nutrition (p<0.01) were significantly more in patients who were operated. Overall mortality for the whole group was 25.4% (14/55) while mortality in PCD only group was 34.5 % (10/29) and in PCD+VARD was 57.1% (4/7).
Conclusion: 63% patients were managed with PCD and irrigation alone. Mortality remained high in patients requiring surgery after extended PCD drainage.
Back to 2018 Program and Abstracts
|