|
Back to 2018 Program and Abstracts
NECROSIS MORPHOLOGY DOES NOT PREDICT SUCCESS OF PERCUTANEOUS DRAIN IN NECROTIZING PANCREATITIS
Thomas K. Maatman*, R. Michael Cournoyer, Sarakshi Mahajan, Alexandra M. Roch, Michael G. House, Attila Nakeeb, Eugene P. Ceppa, C. Max Schmidt, Nicholas J. Zyromski
Surgery, Indiana University, Indianpolis, IN
Background
Minimally invasive methods are increasingly utilized as the first step of treatment in Necrotizing Pancreatitis (NP). Percutaneous Drainage (PD) is often the preferred minimally invasive approach and may provide definitive therapy in up to one-third of patients. Determining the timing and need to "step-up" is more an art than a science. Predictors of success or failure of PD as definitive treatment would streamline treatment algorithms in NP. The aim of this study was to assess the application, predictors of success, and the natural history of PD in NP; hypothesizing that specific necrosis morphology patterns may predict outcome after PD.
Methods
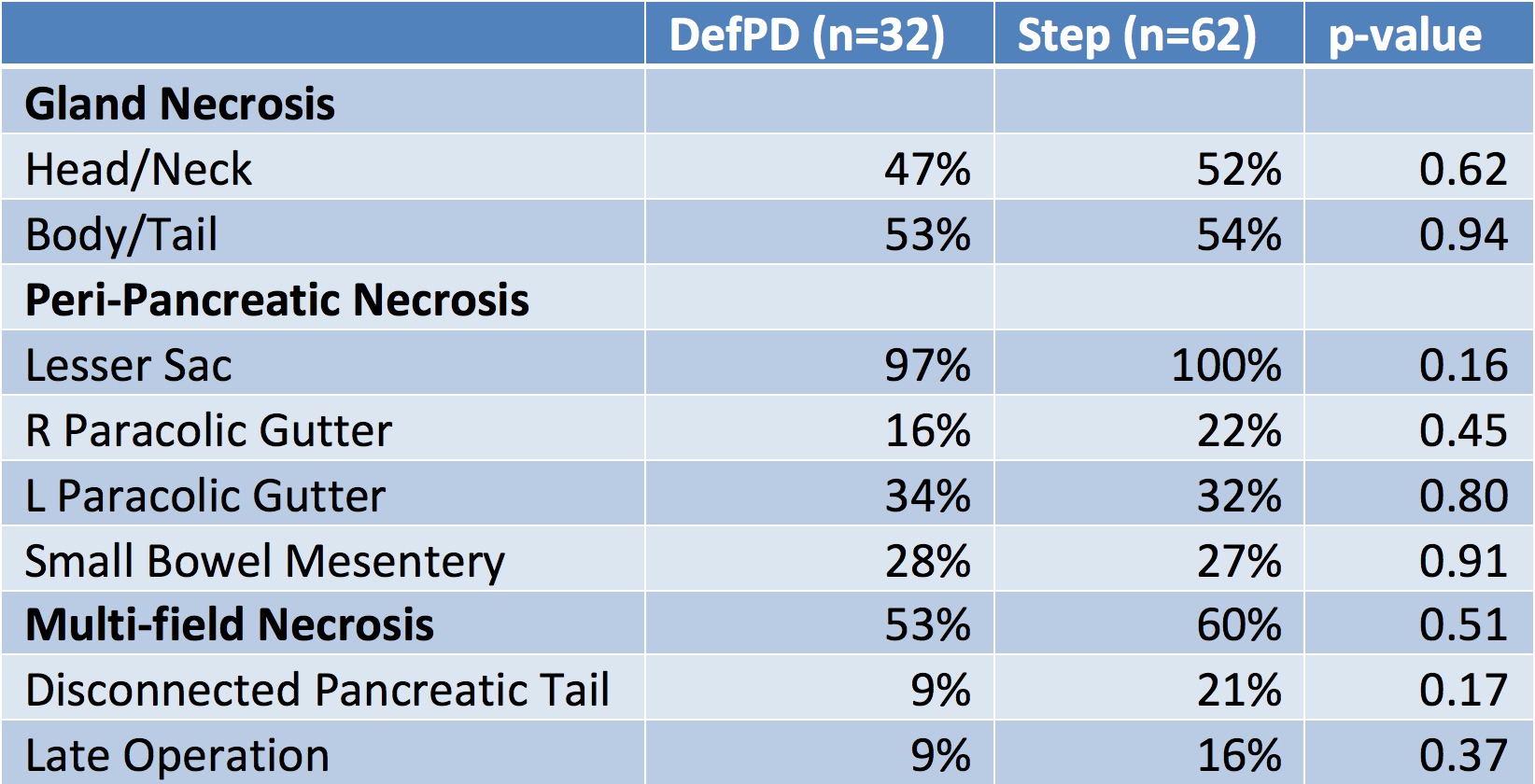
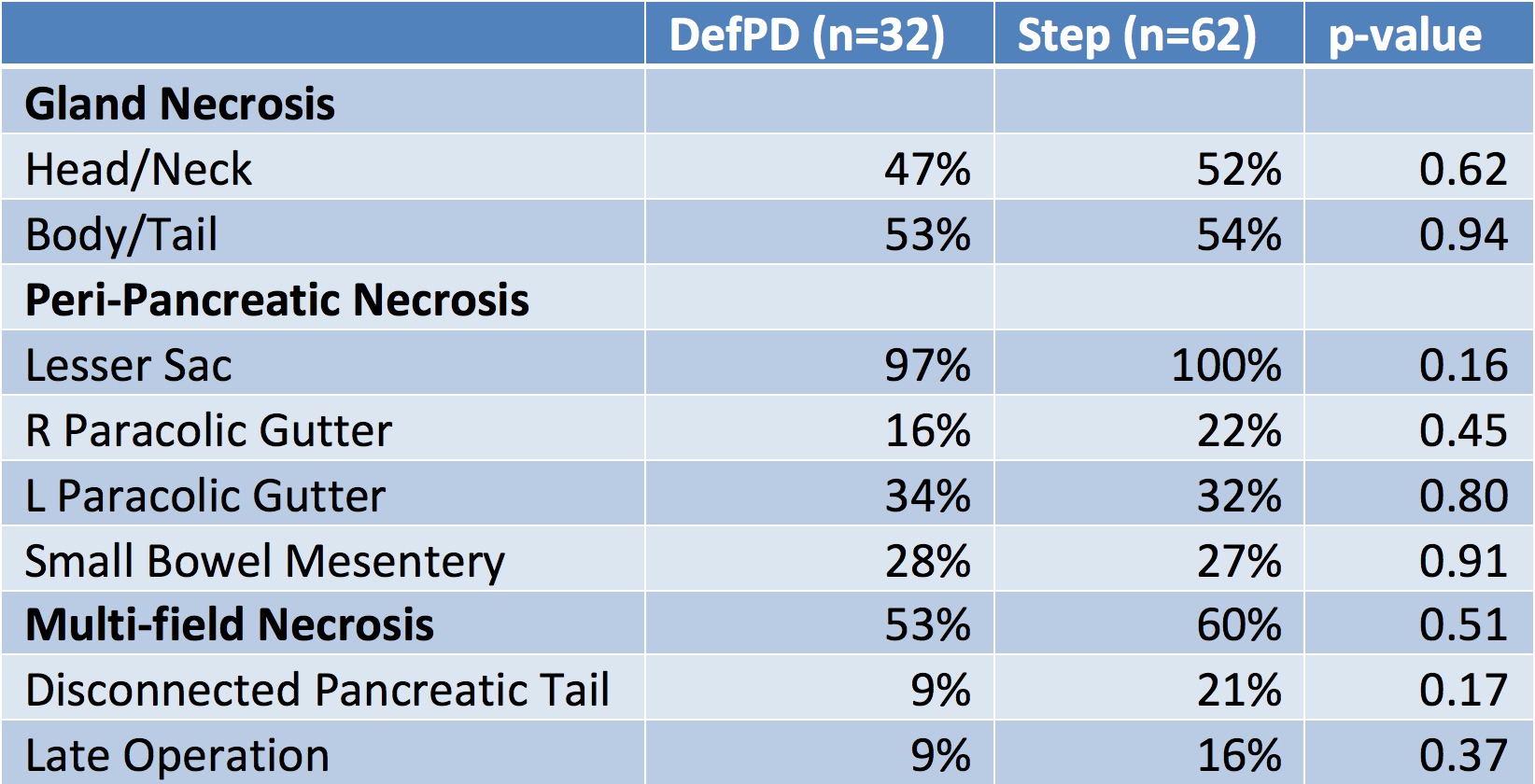
647 NP patients were treated at our institution between 2005 and 2017. Patients undergoing PD as their first intervention were divided into two groups: those in whom PD achieved definitive treatment (DefPD), and those who required step-up to additional intervention (Step). Definitive treatment was defined as removal of all drains with percutaneous drainage as sole management. Cross-sectional imaging immediately prior to drain placement was reviewed and the presence of necrosis was recorded in six locations: head/neck; body/tail; lesser sac; left/right paracolic gutter; and root of the small bowel mesentery. Morphology patterns and outcomes were compared. Independent t-test were performed to analyze the bivariate relationships between the two groups and data points of interests. P-values of <0.05 were accepted as statistically significant.
Results
A total of 107 patients were initially managed with PD: 32 DefPD, 62 Step. Thirteen patients who died prior to disease resolution were censored. Median follow-up was 17 months (range 2-150 months). The necrosis morphology was similar between the two groups (table 1). DefPD required significantly more repeat drainage procedures (3.3 DefPD vs. 2.0 Step, p<0.01). Step-up occurred at a median of 3 weeks. Median time to resolution of disease was similar: 4.8 months (range 1-22) DefPD vs. 5.1 months (range 1-26) Step (p=0.6). Late operation, either distal pancreatectomy with splenectomy or tail pancreatojejunostomy, for disconnected tail occurred in 14% at a median of 15 months (range 4-45 months).
Conclusion
Percutaneous Drainage may act as defintive therapy in a percentage of Necrotizing Pancreatitis patients. Neither necrosis morphology nor presence of disconnected pancreatic tail reliably predict the need for step up in therapy. Long-term follow up is critical, as a significant number of necrotizing pancreatitis patients require late operation.
Back to 2018 Program and Abstracts
|