|
Back to 2018 Program and Abstracts
TOTAL PANCREATECTOMY AFTER NEOADJUVANT THERAPY FOR OPERABLE PANCREATIC CANCER: A CONTEMPORARY ANALYSIS OF THE NATIONAL CANCER DATABASE
Ashley Krepline*, Chad Barnes, Mohammed Aldakkak, Callisia Clarke, Kathleen Christians, Ben George, Paul S. Ritch, Murad Aburajab, Volkan Adsay, Douglas B. Evans, Susan Tsai
Medical College of Wisconsin, Milwaukee, WI
Introduction: Total pancreatectomy (TP) for operable pancreatic cancer (PC) is controversial due to the postoperative morbidity associated with complete exocrine and endocrine insufficiency. Patients with PC treated with upfront TP experience a 15-month median overall survival (OS). We describe the outcomes of patients treated with TP following neoadjuvant (preoperative) therapy.
Methods: The National Cancer Database was queried for patients with pathologic stage I/II PC who received neoadjuvant therapy prior to surgery. Patients were categorized based on the receipt of TP versus pancreaticoduodenectomy (PD). Clinicopathologic characteristics and survival outcomes were compared.
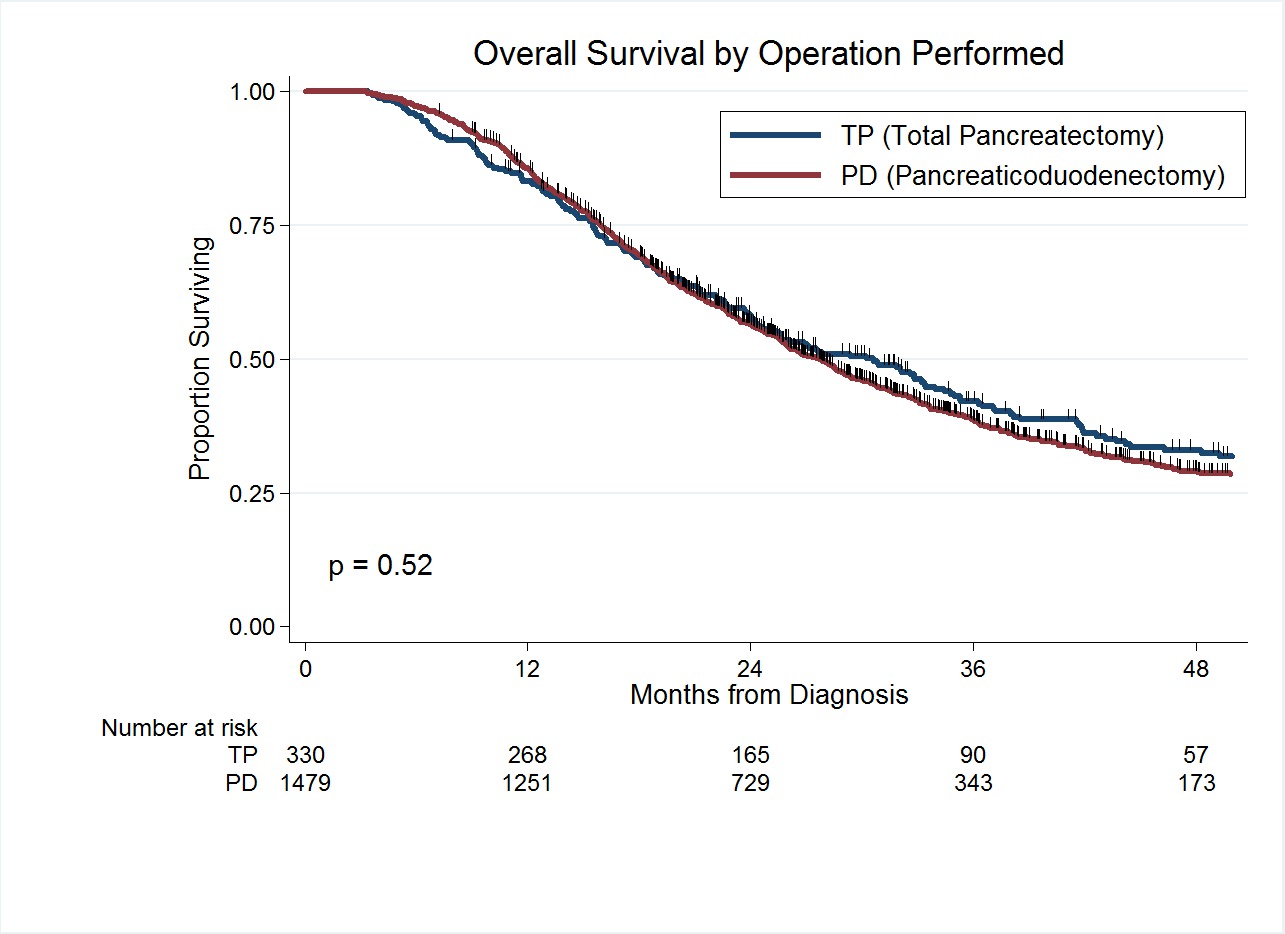
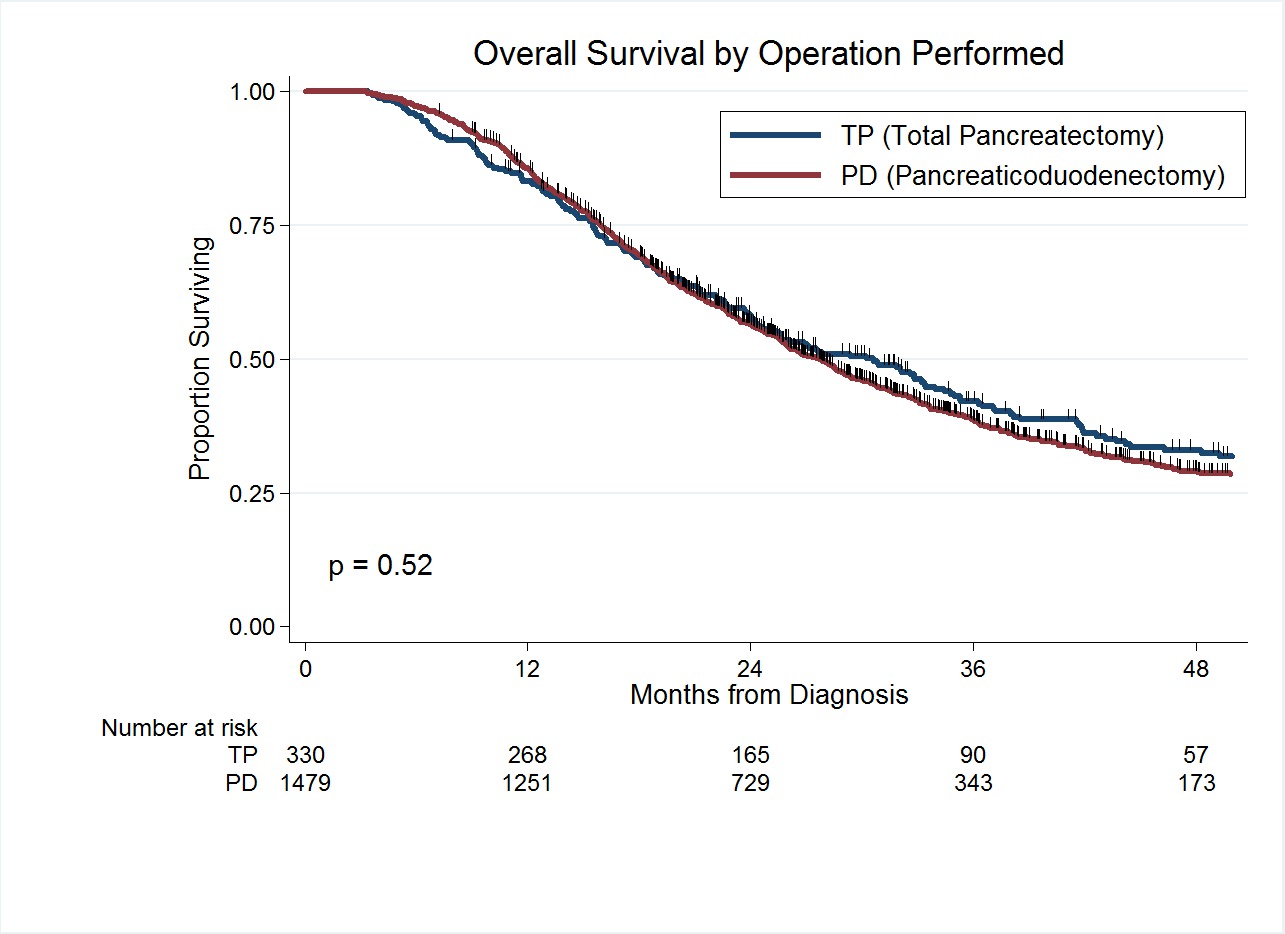
Results: Between 2009 and 2014, data was available for 1,809 (75%) patients who received any form of neoadjuvant therapy and surgery. Of the 1,809 patients, 330 (18%) underwent TP and 1479 (82%) underwent PD. There was no difference in the type of neoadjuvant treatment received or pathologic stage between groups. Median length of hospital stay for TP and PD patients was 9 days and 8 days, respectively (p = 0.03). The 90-day mortality rate was 7% (n=23) for TP as compared to 4% (n=63) for patients who underwent PD (p=0.04). Adjuvant therapy was administered to 118 (36%) of the 330 TP patients and 663 (43%) of the 1479 PD patients (p=0.02). The median OS of all 1,809 patients was 28 months; 31 months for patients who underwent TP and 28 months for patients who underwent PD (p=0.52). The 3-year survivals for patients treated with TP and PD were 42% and 38%, respectively. In an adjusted hazards model, there was no difference in the risk of death between TP and PD patients (HR: 1.10; 95%CI 0.94-1.28; p=0.21).
Conclusion: Following neoadjuvant therapy, TP is associated with a higher 90-day mortality but no difference in long term OS. Notably, the median OS for patients with operable PC treated with neoadjuvant therapy and TP was 31 months - double the median OS reported with a surgery-first approach.
Back to 2018 Program and Abstracts
|