|
Back to 2018 Program and Abstracts
RECURRENCE PATTERNS AND SURVIVAL FOLLOWING PANCREATICODUODENECTOMY WITH PORTAL VEIN RECONSTRUCTION COMPARED TO PATIENTS NOT REQUIRING PORTAL VEIN RECONSTRUCTION
Tarin Worrest*1, Elizabeth Dewey1, Patrick J. Worth2, Erin Gilbert1, Brett C. Sheppard1
1Surgery, Oregon Health and Sciences University, Portland, OR; 2Surgery, Stanford University, Palo Alto, CA
Introduction
Pancreaticoduodenectomy (PD) is standard for resection of pancreatic head malignancies. When borderline-resectable tumor involves the portal system, portal vein reconstruction (PVR) is undertaken to achieve an R0 resection. It is unknown if the need for PVR affects recurrence patterns in pancreatic adenocarcinoma (PDAC). This study compares recurrence and survival in patients who underwent PD with PVR for resection of PDAC to patients who underwent PD alone.
Method
Retrospective review of patients in a prospectively-collected registry who had PD for PDAC from 2007 to 2016. Demographics, tumor characteristics, and chemotherapy information were collected. Initial recurrence sites were recorded based on imaging or biopsy results for the following categories: liver, lung, peritoneum, tumor bed or other. Differences in patient and tumor characteristics between PVR groups was evaluated with chi-square tests. Estimated time to recurrence, disease free-interval, and overall survival (OS) was evaluated with Kaplan-Meier. Significance was set at α = 0.05.
Results
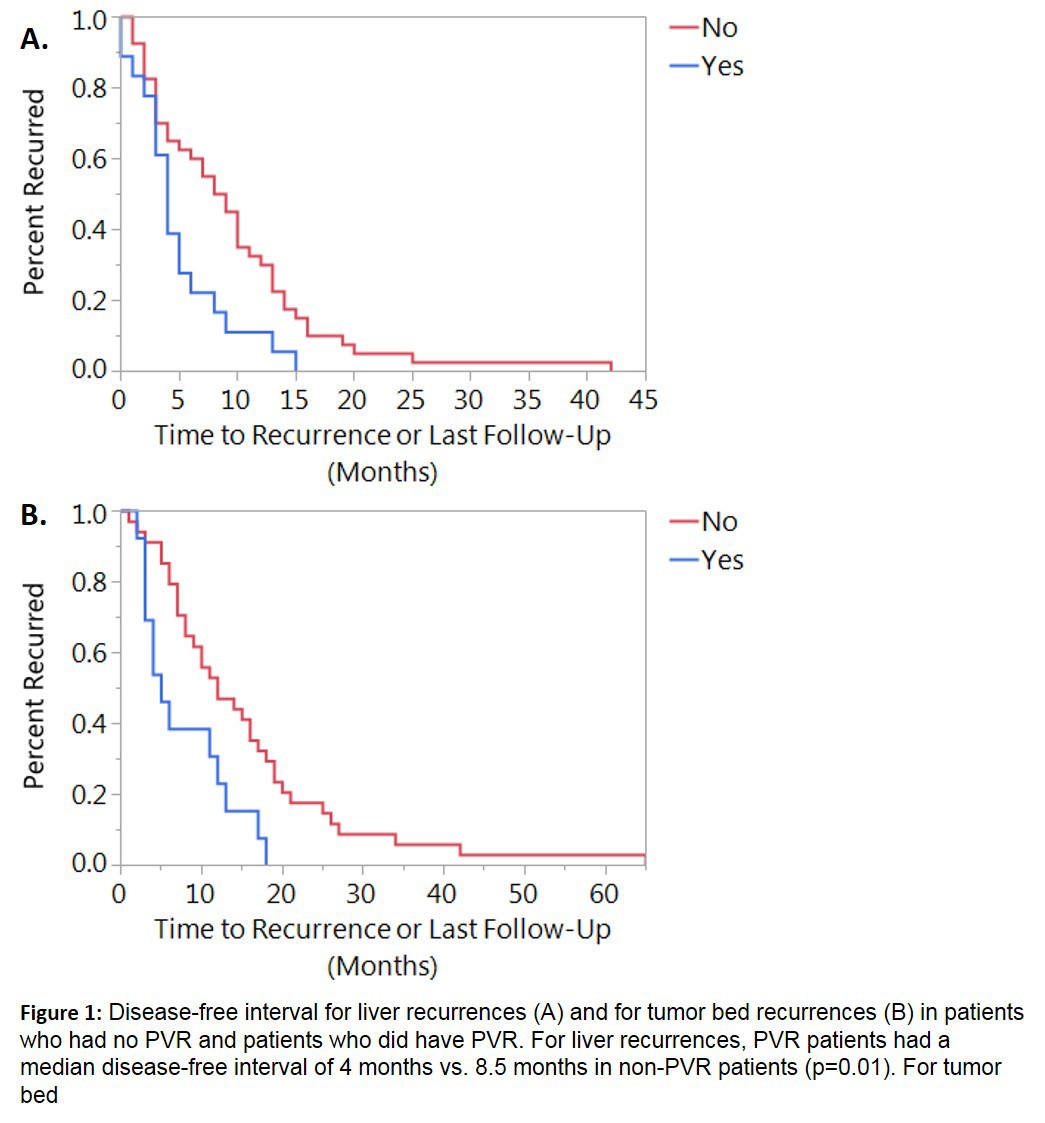
There were 192 PD patients, of which 63 (32.81%) had PVR. Sixteen patients had neoadjuvant chemotherapy, 10 of which required PVR. R0 resection was achieved in 65.1% of PVR patients and 65.9% of non-PVR patients (p=0.86). There was no difference between tumor stage (p=0.64), lymph node positivity (p=0.91), tumor grade (p=0.43), lymphovascular invasion (p=0.24), or perineural invasion (p=0.95). There was no difference in overall number of recurrences (p=0.34). PVR patients did not recur more commonly in any one site. Median disease-free interval (DFI) was significantly different for liver recurrences (PVR 4 months, non-PVR 8.5 months, p=0.01) and tumor bed recurrences (PVR 5 months, non-PVR 12 months, p=0.01, Figure 1). OS was also decreased in PVR versus non-PVR patients with liver and tumor bed recurrences (Table 1). OS for PVR patients was shorter than for non-PVR patients (8 months vs. 15 months, p<0.01).
Conclusion
PVR is equivalent to non-PVR in achieving R0 resection. There are no differences in recurrence rates or location; however, following a recurrence, DFI and OS are shorter for PVR patients. This study, spanning the transition to neoadjuvant therapy, highlights the critical need to optimize neoadjuvant therapy and local control. Improvements in our understanding of the post-therapeutic clonal evolution of recurrent disease will ultimately drive improved outcomes for patients undergoing PD independent of operative conduct.
Table 1
| | Median survival
(months) | 95% confidence interval | p-value | | Lower | Upper | | Liver Recurrence | | | | | | non-PVR | 15 | 12 | 20 | 0.003 | | PVR | 6 | 5 | 12 | | | Tumor Bed Recurrence | | | | | | non-PVR | 20 | 14 | 23 | 0.013 | | PVR | 11 | 5 | 20 | |
Estimated median time to death or last follow up for patients who had recurrences in the liver or in the tumor bed, measured in months. Patients with PVR had decreased survival compared to those that did not. 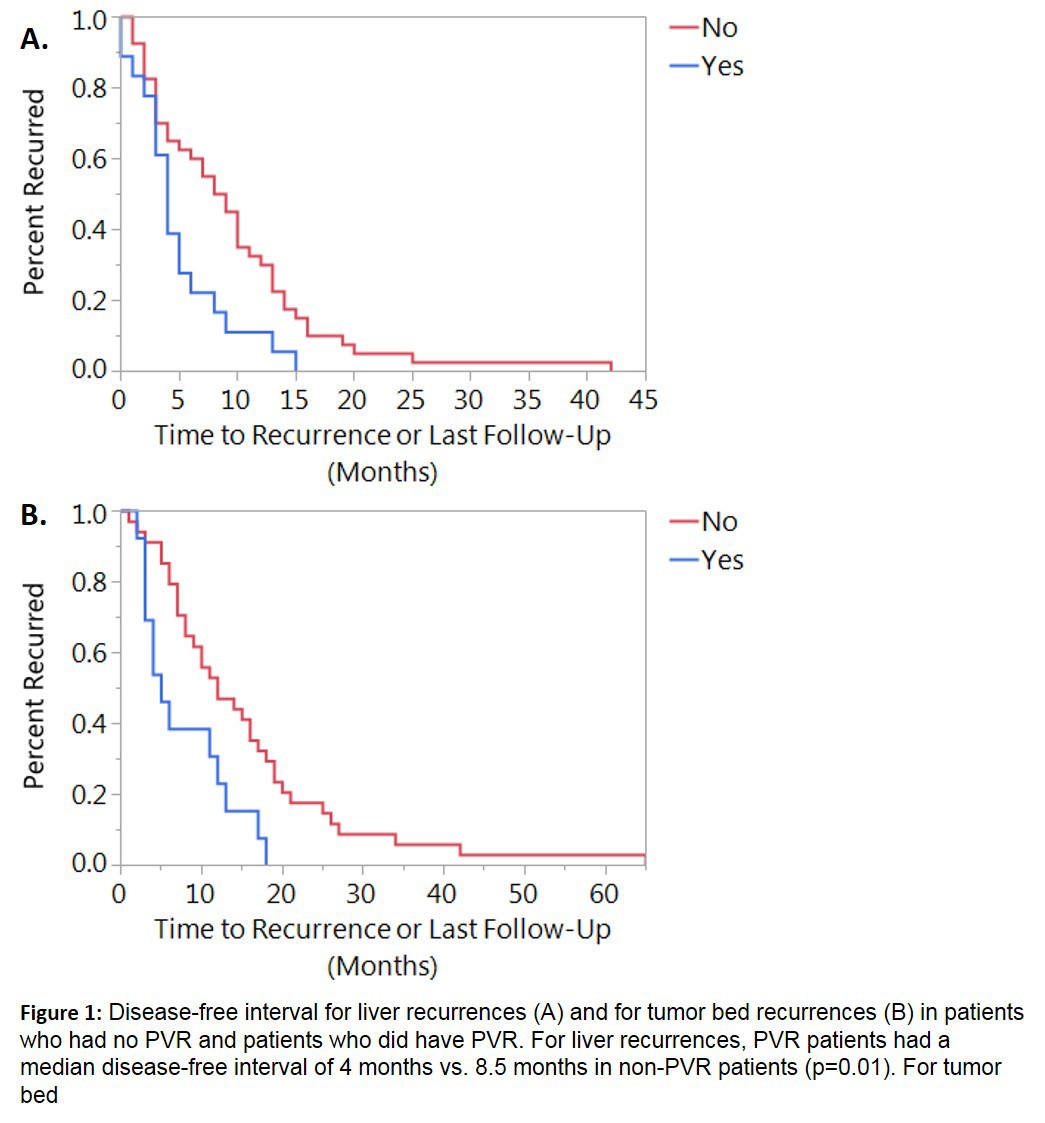
Back to 2018 Program and Abstracts
|